Determining, Declining, and Terminating Medical Treatments
Rick Garlikov
Because modern medicine is better and better able to prevent abrupt and unexpected death, turning it instead into a gradual deterioration and degeneration until the end, getting older, for many people (those who do not die suddenly), is about coming to grips with increasing sorrows and decreasing joys and is about being able to brook more disappointments of ever diminishing, smaller, and narrower dreams and goals, until what is likely left to hope for and to anticipate experiencing is not worth enduring the suffering to wait for it or even to achieve it. Besides trying to avoid that for ourselves, not by dying sooner but by having more to live for longer, we should, as compassionate human beings, combat that happening to others, and especially not contribute to it, even as illness, infirmity, or the wear of time and age takes its physical toll. In other words, we all, as much as reasonable, need to reduce or prevent the psychological and emotional effects of aging, disease, and injury even when we cannot stop the physical ravages of them or heal the underlying condition. In the simplest case, as a bystander one cannot cure someone on crutches, but one can hold the door for him/her or carry something they might be struggling with. Or one can offer to help people in wheel chairs if they want help, as in one older gentleman outside a VA hospital who was having difficulty wheeling his chair up a fairly steep hill. Or you can even have a genuine conversation with someone in a wheelchair instead of averting your eyes and pretending they don’t exist, as many people do. This should be no big deal, but many people avoid such acts of kindness in the face of obvious need and many will even let a door slam shut in front of a person on crutches and pretend not to have seen them, rather than to take a few seconds to hold the door. Others will go out of their way to hold the door or carry the package. But, besides such small acts of kindness, we also need to learn how to talk with and assist in general people who are infirm, disabled, or dying so as to be a source of solace, or at least not an added cause of distress or depression. When I photograph weddings, sometimes a relative is in a wheelchair. In group pictures people don’t mind kneeling down beside the chair to bring themselves closer to the person in it and make the picture look more natural and loving. At one wedding a guest was in a wheelchair and our paths kept crossing. When I had a moment, I asked her what illness or injury had put her in the chair and she said MS. I knew that MS affected the body but not the mind and that it was frustrating simply not to be able to do things one felt like one should easily be able to do, but just can’t. So I looked at her when she said she had MS and said “That is a pain in the ass, isn’t it?!” and it took her by surprise and then she laughed and said “Yes, that is exactly what it is having it.” The unique problem for medicine in regard to reducing the emotional effects of physical deterioration, however, is that some treatments for physiological and physical conditions can risk causing or exacerbating psychological and emotional ones. In some cases biological (or physiological or medical) interventions can even cause more painful or crippling biological harm themselves. This is particularly true for life-threatening and debilitating infirmities, diseases, and conditions where chemical, radiation, or surgical treatments are so severe or harsh that they can readily cause or worsen serious psychological and emotional harms, or even physiological ones. Atul Gawande and the late Paul Kalanithi are two physician authors who have written about this passionately, compassionately, and compellingly in regard to the infirmities of age and to earlier potential ‘end of life’ conditions brought on by severe injury or by untimely illness, not only about their patients, but Dr. Gawande writes about his father’s terminal illness and Dr. Kalanithi writes about his own terminal illness that was diagnosed when he was a neurosurgeon resident looking forward to a most promising career and full life ahead of him. Their books are insightful and beautifully written. But I think there are some things they missed or did not get quite right. This essay is intended to build upon their work and also to put some of their points into a larger, more general context and perspective of moral issues and moral problem solving.[1] Physicians trained to treat physiological problems often find it difficult to refrain from doing so or to consider such self-restraint, even when it would be in the patient’s best psychological and emotional interest not to utilize the potentially most physiologically beneficial treatment. The natural inclination, reinforced by medical education and practice, is to treat the illness or injury (from a biological/medical standpoint) primarily or even solely, rather than the person (from an attending psychological and emotional standpoint), and to seek a cure or improvement, not to let the disease or injury triumph or do any more harm than can be prevented or remedied. Normally treating the disease also treats the patient as a person, or at least does not prevent or conflict with it, since it will get the person back to their desired normal life with only temporary additional inconvenience or temporary additional pain from the treatment. But there are exceptions, notably in the most dire situations, especially now that medicine can save more and more of the body while saving less and less of the person until even vital organs can be kept alive by machine though the person is dead. And an even more clear demonstration of the difference between a person living and his/her organs living is that a person’s organs can be kept alive by transplant into the bodies of others for another entire lifetime even though by then the donor -- person whose organs they were originally -- is clearly long dead. “Doctors in highly charged fields met patients at inflected moments, the most authentic moments, where life and identity were under threat” (Kalanithi, p. 113) “Learning to judge whose lives could be saved, whose couldn't be, and whose shouldn't be requires an unattainable prognostic ability. I made mistakes. Rushing a patient to the OR to save only enough brain that his heart beats but he can never speak, he eats through a tube, and he is condemned to an existence he would never want ... I came to see this as a more egregious failure than the patient dying. The twilight existence of unconscious metabolism becomes an unbearable burden, usually left to an institution, where the family, unable to attain closure, visits with increasing rarity, until the inevitable fatal bedsore or pneumonia sets in.” (Kalanithi, p. 80) “The problem with medicine and the institutions it has spawned for the care of the sick and the old is not that they have had an incorrect view of what makes life significant. The problem is that they have had almost no view at all. Medicine’s focus is narrow. Medical professionals concentrate on repair of health, not sustenance of the soul. Yet—and this is the painful paradox—we have decided that they should be the ones who largely define how we live in our waning days. For more than half a century now, we have treated the trials of sickness, aging, and mortality as medical concerns.” (Gawande, p. 128) When “repair of health” enhances “sustenance of the soul”, there is no conflict between them. The problem arises simply when the two conflict, particularly when the conflict is not recognized or when repair of health is assumed with no or little doubt to be the more important or essential and determining factor. Much of modern medicine borrows useful time from the present with the hope of paying it back with interest, great or small, in the future. It is a specific kind of deferred gratification and investment in the future[2]. Restrictive diet, activity, even bedrest, surgery, chemo, radiation, or pain now is meant to make a greater amount of, and more satisfying, activity possible in the future. One fundamental difficulty in determining which treatments are worth the patient’s undergoing, however, is in not being able to divine the future with total accuracy, and so we have to use probability and educated guesses about what is reasonable to borrow and what the payback will be, and what is worth risking borrowing to get what possible return. The science of medicine is not precise, and therefore the utility and actual benefit or harm of treatment options is not certain. Consider one example by Dr. Gawande about one of his patients: “Surgery offered her the possibility of being able to eat again and a very good likelihood of controlling her nausea, but it carried substantial risk of giving her only pain without improvement or adding yet new miseries. She had, I estimated for her, a 75 percent chance I’d make her future better, at least for a little while, and a 25 percent chance I’d make it worse. So what then was the right thing for her to do? … how do you weigh relief from nausea, and the chances of being able to eat again, against the possibilities of pain, of infections, of having to live with stooling into a bag?” (p. 236) Ethical and practical judgment always needs to weigh the probabilities of the different options available along with the value in general and the significance to the particular person affected by the possible results of each. In medical cases the most important consequences to consider are primarily, but not solely, those to the patient and secondarily to the patient’s family and loved ones, particularly those people who may also need to be caregivers or who may suffer collateral damage from the resulting needs of the patient and the emotional, physical, and financial resources devoted to trying to meet them. For example, when a neonate is saved merely biologically and consigned to a likely future of mere breathing and drooling, unable to move, eat, or to sit up by itself, and with no discernible emotional reactions to any stimuli, that takes a severe toll on the family and particularly on siblings even if they are compassionate, caring, understanding, and loving. Except that the stakes are higher and the consequences more important and significant, making these kinds of medical decisions is like trying to balance any other important costs and benefits for making choices based on probabilities and (sometimes vaguely known or conflicting) values, such as when it is worth an expensive repair job on an old car or whether it is better instead to spend much more money for a new one less likely to break down and which might be somewhat safer or have more features, even though you also hate to be wasteful or extravagant, but would kind of also like a new car (though you know that excitement wears off soon, and also brings more worries about its being hit or dinged in a parking lot, etc.). Or consider whether to take a job that pays less now but has potentially greater, but less certain, financial reward compared with one that pays more now, or whether to take a higher paying job with more stress and less personal satisfaction or one that is more personally rewarding, but financially dismal or discouraging. If you knew precisely what the results would be of the different options, it would sometimes be an easy choice. E.g., if you knew a $2,000 repair of your car was going to lead to another different $8,000 breakdown in three months, and then a $5,000 other problem six months after that you would be more reasonably inclined to buy the new car. But if you knew the car would run well for five years after the current $2,000 repair, that would be the much more economical choice than buying the new car now. If you knew that the job that was more personally rewarding would also end up being far more lucrative, again that would be an easy decision. In the surgery case above, if the outcome was 100% certain in either direction, it would be an easy decision (assuming the surgery was easily affordable – by the patient, a benefactor, or insurance -- and would be successful). [Coincidentally just after typing this I received mail that says my own long-term care policy will be raising its monthly premiums 30% and I need to choose between paying that increase or decreasing the benefits. They even offer allowing what has been paid so far to be used as a benefit for long term care payments if I were choose that option and quit paying further premiums. What I have paid so far would cover maybe 4 to 8 months of in home or nursing home care at the projected costs they say those run where I live. Basically they are using actuarial data to keep their policies solvent and profitable for them, playing the overall population odds the way any large enough gambling institution (from a lottery to a racetrack to a casino, or any insurance company) can practically guarantee profits for itself, despite having to make large payouts to some customers; i.e., those who win at gambling for money and those covered by insurance who lose life, health, or property. But the individual betters/customers have no way to make sure they are choosing the best option for themselves because they can only take into account probabilities and possible costs to themselves, not knowing what is actually going to happen to them. Clearly, if you knew you would die suddenly without need for long term care, you would not pay (more) premiums for it; and clearly if you knew you would need a great deal of expensive long term care, you would buy the longest policy with the most benefits you would need.] However, 100% certainty is not always the determining factor. If you knew for certain that you would like one job less than another but make more money at it, you then have to try to decide how important or significant to you the more money with less job satisfaction is to you rather than the reverse. That may not be an easy decision. If you knew surgery would improve your digestion but increase your care needs and possibly decrease your mobility, that would still be a difficult decision. If you knew that a treatment would increase your lifespan a certain amount but decrease the quality and activities you enjoy, it would still be a difficult decision, particularly when you get conflicting advice from people or advice that conflicts with your own intuitive predilections and are not sure you can make up for your losses with new joys, or not miss them as much as you think you will. There are various trade-offs outside of medicine that we often have to decide between, sometimes they are exaggerated for humor, as in the view that eating healthy will give you a longer, healthier life but one in which you never get to enjoy a good meal, or where a good meal is your last one and is an item at the end of your ‘bucket list’. Tom and Ray Magliozzi, in their typical pointed and irreverent way on their NPR radio program Car Talk, once proposed their theory of why exercise was not a good or worthwhile thing, because they suggested it only added the amount of time you spend exercising to your longevity – meaning that each hour of exercise added exactly one hour to your life – which effectively turned time in your younger years that you had the ability to do something really interesting with but didn’t because you were exercising, into time in your later years when you were more likely unable to do anything useful with it. Of course, if you have a form of exercise you really enjoy (running or playing an active, muscle and cardio enhancing sport), then their theory does not apply, since you are doing something you like and extending your life while and by doing it. In real life, Jacqueline Kennedy Onassis is reported to have said when she found out she had non-Hodgkin's lymphoma that if she had known she was going to die from it in her early 60’s, she would not have done all those sit-ups. Now, many health care professionals and many patients have long known that some treatments, and even some cures, are worse than the diseases or conditions for which they are used or might be used. They see the conflict between repair of health and sustenance of the soul. That is more easily seen when none of the options likely include the patient’s death or (further) permanent and serious disability. More aggressive treatments seem to be warranted for more aggressive illnesses or injuries, but that is not necessarily the case. Instead there is some intuitive notion we have about what is worth treating with what means, not because the condition is aggressive or not, and not because the treatment is aggressive or harsh or not, but about whether the treatment is worth enduring in order to improve or remedy the condition. That intuition may not be correct and may be changed by persuasion and evidence, but it is generally the starting point. As a teen, I developed a reddish-brown patchy skin condition on parts of my back and stomach, under my arms that a dermatologist diagnosed as tinea versicolor. At that time, the standard medical treatment was a sulfur solution which was to be applied after a shower. I dutifully applied it, and it smelled terrible, so consequently I smelled terrible. I really did not want to go to school smelling like that. So I went back to the dermatologist and asked whether the skin condition was dangerous or contagious or would spread all over my body, etc. He laughed and said “Why, is the treatment worse than the disease?” And I said, yes, it was. He expected that and said it would be okay not to treat it. So I didn’t. Had it been important to treat it and had he explained why, I was amenable to using the treatment and trying to work around it socially somehow. Years later, there was a much better treatment – more effective and odor free, but that will be another story in a different context later. And then subsequent to that later treatment, which was a cream, there was a pill that could be taken, and I filled that pill prescription at the pharmacy, only to find out from the packaging information that in 1 in 10,000 cases the medication caused severe liver damage. I preferred the cream, which was very effective, and even having to keep the spots if there were no effective cream, to risking serious liver damage, even if the odds had been better against getting liver damage from the pills. I threw the pills away without taking any. It can be argued it is also true, but just not as obvious, that the treatment can be worse than the disease even when the disease is terminal and will be fatal. For there are worse things than death and worse ways to die than from natural causes or even from falls or other solo accidents in less than optimally safe conditions, even when nature can be brutal in its own way. Dr. Gawande and Dr. Kalanithi understand that, but it is not known by all, and the idea is often lost in the pressure to want to ‘help’ the patient medically and save his/her life. That pressure is on the doctor but it also is on the patient from loved ones[3] and from physicians who don’t understand the significance to the patient of a life without certain abilities and freedoms important to him or her. An older friend of mine, who was a retired physician was diagnosed with bladder cancer, the treatment of which at the time was Draconian and not likely successful. It might even shorten his life. His family and his physician were urging him to take the treatment in the remote hope of saving his life. He asked me what I thought, and I had him tell me the medical pros and cons, and the relative values to him of each, addressing all challenges I had to any of his intuitive preferences. Working his way through that conversation helped him confirm his initial intuitive preference he would prefer to die from the cancer, with palliative care if and when necessary, than to suffer the treatment that didn’t give enough odds of success to make it worth trying and that had a likely chance of making him suffer more. He had had a very good life as a pioneering public health physician and still active member of the community where he lived, and, though he had not made a lot of money in that branch of medicine, his effects were in order for his wife and grown children who were provided for financially, and he preferred not to be medically ‘tortured’ along with dying from cancer if he was likely to die from the cancer anyway. He didn’t have a bucket list that was any different from his normal ‘list’, and he had pretty much accomplished the things open to him that he had wanted to do. He didn’t, of course, prefer to die, but he was prepared to. When he became progressively weaker, he did write a beautiful farewell letter to his family and friends that he asked to have read at his funeral, along with the closing prayer he wanted recited. Dr. Gawande’s father, also a physician, with a growing tumor in his spine pressing against his spinal cord faced the same kind of dilemma: We needed guidance. He was torn between living the best he could with what he had versus sacrificing the life he had left for a murky chance of time later. One of the beauties of the old system was that it made these decisions simple. You took the most aggressive treatment available. It wasn’t a decision at all, really, but a default setting. This business of deliberating on your options—of figuring out your priorities and working with a doctor to match your treatment to them—was exhausting and complicated, particularly when you didn’t have an expert ready to help you parse the unknowns and ambiguities. The pressure remains all in one direction, toward doing more, because the only mistake clinicians seem to fear is doing too little. Most have no appreciation that equally terrible mistakes are possible in the other direction—that doing too much could be no less devastating to a person’s life. (Gawande, p. 220) The kinds of pressures others put on you and that you even put on yourself in momentous, life-determining choices come up at other times also – people urging you to get married (at or by a certain age or to a particular person), to change jobs, move to a different state or country for a much better possible opportunity, invest in some enterprise, have a(nother) baby, move in with grown children (or conversely, take care of elderly parents) or enter (or put parents in) assisted living or a nursing home, etc. All these are peer and internal pressures, whether conscious or subconscious, to conform to psychological and cultural norms, which too often are simply unquestioned, let alone unchallenged. And just as medicine tends to want to do more medically/physiologically for, or to, the patient, institutions for the elderly or otherwise disabled also tend to focus on physical safety even if that robs people of a lifestyle that is far more meaningful and significantly important to them. Dr. Gawande devotes many pages to pointing out that is an error. And he could have also added to the statement above, by saying “This business of deliberating on your options—of figuring out your priorities and working with a doctor and with those setting you up in living quarters to match your treatment and desired lifestyle to them—was exhausting and complicated, particularly when you didn’t have an expert ready to help you parse the unknowns and ambiguities.” However, Dr. Kalanithi, I think, puts too much stock in the patients’ figuring out or already knowing themselves what they really want. I think patients need more help with that, part of which involves knowing what is medically possible and more or less likely or reasonable, and knowing what choices other patients have made in the past and how satisfactorily or unsatisfactorily those turned out for them – not simply in terms of medical results but in terms of whether it was really what they wanted afterward even if it did go well medically. He writes, on pp. 165-166: “I could hear Emma’s [his oncologist] voice again: You have to figure out what’s most important to you. If I no longer sought to fly on the
highest trajectory of neurosurgeon and neuroscientist, what did I want? I didn’t know. But if I did not know what I wanted, I had learned something, something not found in Hippocrates, Maimonides, or Osler: the physician’s duty is not to stave off death or return patients to their old lives, but to take into our arms a patient and family whose lives have disintegrated and work until they can stand back up and face, and make sense of, their own existence. … Emma hadn’t given me back my old identity. She’d protected my ability to forge a new one. And finally I knew I would have to.” I will explain shortly why I don’t think that is sufficient. Although both Dr. Gawande and Dr. Kalanithi are trying to take medicine further in these kinds of cases than many physicians are comfortable going, I think physicians need to go even beyond Dr. Gawande’s and Dr. Kalanithi’s goals, though not necessarily on their own if they are not themselves interested in pursuing the knowledge to do it, but with experts in a field (that will have to be new) specializing in these sorts of decisions to help patients and doctors make them wisely. Physicians who do not want to take on this kind of task or feel they could not learn to do it adequately or well, shouldn’t have to. They have sufficient work to do attending to people’s medical needs in terms of “repair of health”, and there are other people physicians could refer the patient to who can help the patient make a decision. The physician should, however, provide the patient with at least the medical/physiological/biological consequences and their rough probabilities of the different treatment options. And although Dr. Gawande believes that the physician needs to help guide the patient in determining what s/he really wants and together choose the treatment options most likely to make it achievable, he puts too much stock in particular, limited ways to determine how to do that – 1) the concept of “second-order desires” and 2) using Daniel Kahneman’s theory of peak-end experiences, which states “people judge an experience largely based on how they felt at its peak (i.e., its most intense point) and at its end, rather than based on the total sum or average of every moment of the experience. The effect occurs regardless of whether the experience is pleasant or unpleasant.” (https://en.wikipedia.org/wiki/Peak%E2%80%93end_rule) I will explain about “second-order desires” shortly, but will begin with the theory of peak-end experiences, which on the surface has a certain plausibility, but which I don’t think will be very helpful in end-of-life cases, and which I think Dr. Gawande mistakenly believes he is using, instead of what he is really considering, in the case where he expressly said he applied it. Dr. Gawande explains some of Kahneman’s work in studying patient’s experiences about unpleasant medical procedures, such as colonoscopies and kidney stone procedures while awake: “Our natural assumption is that the
final ratings by patients would represent something like the sum of the
moment-by-moment ones. We believe that
having a longer duration of pain is worse than a shorter duration and that
having a greater average level of pain is worse than having a lower average
level. But this wasn’t what the patients
reported at all. Their final ratings
largely ignored the duration of pain.
Instead the ratings were best predicted by what Kahneman termed the
‘Peak-End rule’: an average of the pain experienced at just two moments -- the
single worst moment of the procedure and the very end.” (Gawande, p. 237) Dr. Gawande then points out that watching your favorite team play well all game but blow it at the end basically retroactively ruins the whole experience for you even though you had hours of happy excitement and only the ending minute of misery. Here again, Dr. Gawande is focusing on a negative experience. But the theory applies in the same, but opposite way, of course to the other team and its fans, since the victory makes them thrilled and makes them not care at all about the hours of agony they went through being behind and having to anticipate defeat. And he then tries to apply the theory to patient care and decision-making about treatment, but in a way, I don’t think really works or is necessary at all: “If the remembering self and the
experiencing self can come to radically different opinions about the same
experience, then the difficult question is which one to listen to. This was [his patient’s] torment at bottom,
and to a certain extent mine, if I was to help guide her. Should we listen to the experiencing self,
which would likely have a lower average amount of suffering in the time to come
if she underwent surgery rather if she just went home – and might even get to
eat for a while again?” But she “didn’t
know if she was willing to face the suffering surgery might inflict on her and
feared being left worse off. ‘I don’t want to take risky chances,’ she said,
and by that, I realized, she meant that didn’t want to take a high-stakes
gamble on how her story would turn out.” (Gawande, p. 238) He knew from her accounts that the small joys she was having with friends and family that if she could just continue that a while longer, it would be preferable to her than taking a chance to eat again if taking that chance could turn out to mean not being able to do those things. I don’t see how this relates to or derives from the peak-end theory of remembering, which after all is different from experiencing something at the time, both of which are not necessarily the same as the anticipation of an experience. For there is not only experiencing of the present and memory of the past, but anticipation of the future. And these may or may not be the same. One can dread anticipating an experience that turns out to be not that bad and that is remembered even as being good. College and war are two different kinds of major formative experiences people have that they tend to fear or dread beforehand, muddle through during, and then remember as having been significant good forces that matured them and made them what they are happy to be today. There are, of course, exceptions in that some people look forward to college and there are perhaps even some people who look forward to going to war and being able to serve their country in that way, possibly even if they were to die, or perhaps having faith or confidence they won’t. College or war may turn out not to live up to the anticipation. And there are people harmed or broken by war. And of course if one is killed in war, there is not the victim’s remembrance of it. And since the peak-end theory is about what we remember, as
opposed to what we experience (or anticipate), it is not clear it applies at
all to end-of-life cases. It is their
anticipation and actual experience at the time that matters, not their memory
after death. Insofar as the peaks and
valleys matter, end of life experience and anticipation of it can have
those. But they won’t have anything to
do with memories after death, other than memories by friends, loved ones,
medical staff, etc. What Dr. Gawande wrote about going through the decision process in the above case is: For human beings, life is
meaningful because it is a story. A story has a sense of a whole, and its arc
is determined by the significant moments, the ones where something happens.
Measurements of people’s minute-by-minute levels of pleasure and pain miss this
fundamental aspect of human existence. A seemingly happy life may be empty. A seemingly
difficult life may be devoted to a great cause. We have purposes larger than
ourselves. Unlike your experiencing self—which is absorbed in the moment—your
remembering self is attempting to recognize not only the peaks of joy and
valleys of misery but also how the story works out as a whole. That is
profoundly affected by how things ultimately turn out. Why would a football fan
let a few flubbed minutes at the end of the game ruin three hours of bliss?
Because a football game is a story. And in stories, endings matter. (Gawande, pp. 238-9) But in end-of-life cases, the story ends with death. In all our lives, the story ends with death – at least the physical or biological story. And while the patient may have memories as s/he goes along toward the end, aren’t the experiences and perceptions of them at the time at least equally, if not more, important? Dementia patients may not even have memories one way or the other of their experiences, but aren’t those experiences important while they are having them anyway? In fact, aren’t experiences, particularly good ones, in life important to have even if one cannot remember them or even if one faces oblivion after death that blots out all memory. Isn’t it at least as important to have a life well lived as to have memories of it? Obviously, having good experiences and remembering them is better than not remembering them, but having them and not remembering them is still better than not having them at all. At least one had them in the moment. The above patient was able to reveal to Dr. Gawande in the conversation he refers to what she would like to be able to anticipate and experience, not what she wants to remember at the end of the story. At the end of the story, she will have died. Insofar as savoring a past event requires memory of it or reliving it in some way, she would like to be able to do that too, but the emphasis is on what she wants to happen, not what she wants to be able to remember having happened at the end. She was stating her preferences about how she would like to spend the rest of her time she had left and what joys she would like to be able to experience, even if that meant having shorter time left to keep having them. She wasn’t looking for a good ending but the best experiences left for her, and she wasn’t seeking peaks but things that, as he refers to elsewhere with his father, days and moments that were ‘good enough.’ Moreover, while it is tempting to believe in the adages “All’s well that ends well” and “Any airplane landing everyone can walk away from is a good, successful landing” it is not always true, or Churchill’s variation on them that “Nothing in life is so exhilarating as to be shot at without result.” (Churchill 1898) Even without any particularly memorable valleys during an experience, a successful conclusion to it does not make it remembered as a good one. Some experiences are ordeals that wreak havoc on people for reasons other than any particular memorable incident in them. War is one such experience, even if one survives it uninjured. And experiences can cause post-traumatic stress even about things that never happened but which could have happened and that one feared or had anxiety about. Some PTSD is about things that did happen to the sufferer, but other PTSD attacks are about what might have happened but just fortunately did not. Or if one is acquitted in a trial of a crime one did not commit, the experience of having to have a lawyer and defend oneself in court can be devastating even though it turned out well. One should still not have had to go through it. A computer crash is always disheartening, even after all the data and software are restored or replaced. Even buying a new and better computer is not a happy experience because it can take a long time to set up and transfer all your data and software to. It is a laborious process just to get back to where you were. In some of these things what is so disappointing or devastating is not what happened, but what didn’t happen because of the ‘opportunity costs’ – the lost opportunities from contending with what did happen. Time and energy were wasted, frustration and fears felt, joys missed. Freedom does not make one forget slavery nor does divorce let one forget an unhappy marriage, even if there were no particular memorable bad incidents in it. Getting a good job does not erase the taste left by having had a bad one. Plus, while it is often true that many people find the end
of a story to be an important, or even the most important, part of it, not
everyone feels that way about every kind of experience and one doesn’t always
have to. It depends in part on what you
expect or hope to get out of an experience and in part on your interpretation
of an experience before and after you have it – sometimes even while you are
going through it. In the 1975 World Series between Boston and Cincinnati,
game 6 was a titanic extra-inning battle that each team had various chances to
win that were thwarted by excellent play by the other side. If Cincinnati
won the game, they would be champions; if Boston won the game, the series would
go to game 7. Boston won on the barely fair home run by Carlton Fisk in
the bottom of the 12th inning. Prior to game 7, Pete Rose, one of
baseball's most competitive players ever, was asked about the disappointment of
losing game 6 and whether it could be shaken off to play game 7 at one's best
or whether it might prove so demoralizing as to cause them to lose before they
even took the field. Rose enthusiastically and immediately said it was
difficult to be disappointed in the result, given that the pride and honor in
having played in what might have been one of the best and most exciting,
skillful, and competitive games in World Series history far outweighed
that. To have just been a part of that game was tremendously exciting, he
said, nd no matter what happened in game 7, he and his teammates would always
have that. Clearly the result or “end” of game 6 did not ruin the
experience of it for him. Cincinnati did go on to win game 7
and thus the World Series that year, but he didn’t know that would happen when
he said what he did. That kind of
perspective should be taught to children, but too often is not. And it
must be pointed out that if the only thrill in sports is to be winning,
particularly championships, then that automatically makes every season one in
which most players and fans will be disappointed, which is rather a stupid and
contradictory, self-defeating pursuit. "Sure, let's devise an
activity where the thrill of it is denied to most of the people who do it and
most of the people who follow it. That should be fun, exciting, and
really popular." In a less momentous and less public
circumstance, my older daughter had another one of her annual violin
performance judging events that in the past she had dreaded before and hated
during and after. By then she was in
sixth grade, and her English teacher that year required them to keep a
journal. My daughter did not have
performance anxiety, and in fact she volunteered to give violin and piano
performances in her school; she enjoyed playing for others. What she hated was being graded on it, being
judged. I had always felt bad about her
teacher making her perform for these ‘competitions’ or contests or whatever
they were, and finally I told my daughter that if she didn’t want to do it, she
didn’t have to. I would just take her
home if she wanted to leave without playing and deal later with the teacher
about it. She surprised me by saying
“No, this is okay, because it is going to make a really good journal entry no
matter how it goes.” She was focusing on
the experience, not the outcome or ‘end’, and the experience of playing and being
judged didn’t have to go well for the larger, or more important outcome or
experience for her – having an interesting journal entry to write. I don’t even know whether the journal entries
were graded or not or whether she cared about the grade if they were. Also, we often have an overall
feeling of achievement when there is no particular ending to an activity or no
specific memories of moments in it. I
used to love studying algebra on my own after school, and read ahead in the
book, working problems to see whether I understood how to do them correctly or
not. And I used to love hitting tennis
balls against the practice wall as I tried to improve at tennis. And I loved playing tennis, but more for the
exercise and fun than for any particular wins or losses. Sure, some swings or shots were better than
others at tennis, some matches stand out for particular reasons, but not so
much for the win or loss, but for something memorable and odd or important in
them that couldn’t be classified as peaks or valleys, and some problems in
algebra were more difficult and thus more rewarding to solve, but I recall few,
if any, particular shots even in memorable tennis matches and few algebra
problems even in good self-study sessions.
Dr. Gawande even points out some enjoyable aspects of playing tennis
with his father that don’t have to do with who won or lost or have particularly
memorable points, but with style of play: “Whenever I came home, I’d bring my
tennis rackets and we’d go out on the local courts. He played to win, and so did I. He’d drop shot me; I’d drop shot him. He’d
lob me; I’d lob him.” It was the zest,
vigor, and competitive tenacity with which they played, particularly his
father, that he seems to most remember and appreciate, not the outcomes or any
shot or point during their matches.
I do recall one algebra problem
fondly even though, or because, it made a fool out of me in a way that was
interesting, and I spent hours and hours working it out though it should only
have taken a second. The problem was one
of those “a train leaves New York for Los Angeles at some time and speed, and
then a while later, one leaves Los Angeles for New York going a slightly
different speed”. The speeds and times
given were precise and not easily compared.
There was something like a 13 hour and 43 minute difference between
their starting times and their speeds were some unusual number and fraction
apart, like maybe 19.64 mph or some such.
You had to work out when they passed each other which would be closer to
New York. I mistakenly took that to mean
the usual “where will they meet and will it be closer to New York or to
LA?” Trying to solve that question took hours and hours, and
I had to resort to changing the problem to speeds and times I could more easily
work with to see how to go about calculating the answer to such a problem. After I worked it out with the easier numbers
I went back and applied the method to the difficult numbers they gave. It turned out, to my surprise, that the train
that left New York was the same number of miles from New York as was the other
train that had left Los Angeles. I
thought that odd, and changed the speeds and departure time differences to see
what would happened then. It turned out
that although it gave a different distance from New York, again the train that
left New York was the same distance from it as was the train that left Los
Angeles. Now that seemed really odd, and
so I set out to find out how that was happening. How could it be that apparently no matter what
their speeds or departure times, they ended up the same distance from New York
as each other, no matter where that was.
After pondering even that for longer than I should have, it finally
dawned on me what is probably obvious to you from the beginning – that wherever they pass each other, they will
then be together and therefore of course the same distance not only from New
York as each other, but the same distance from Los Angeles (or Timbuctoo or the
moon) as each other too. I was at once
ashamed I hadn’t thought of it right away (or even anywhere near the middle or
end), but proud I had worked it out the hard way I did. I still find it amusing to think about. There are other problems that are
stated in ways to make them seem more difficult than they are[i]. What is cool and memorable about these
problems has nothing to do with whether you solve them or not (and one usually
doesn’t solve them) but how cleverly they are constructed to fool you and how
you fall for it or see it so as not to fall for it. Unless you are arbitrarily and trivially just
going to define any memorable aspect of an activity as being a peak or valley
in it, the memorable aspects of those activities will not necessarily be what
one might consider a peaks or valleys in them.
One of the things I and my college classmates used to dread was going to
check on our freshmen chemistry exam scores.
You had to climb four flights of stairs to get to the professor’s door
on which he had your exam grade posted by your student ID number or some
such. The pit in your stomach and the
fear was palpable on each step, and that feeling did not go away even if you
were relieved to find you had passed or even got an A. And there was no peak or
valley during the walk to the building and the climb of the stairs. The whole
experience was simply nerve-wracking and terrifying because you (usually
mistakenly) felt your whole future was on the line (and you would be, or have
been shown to be, a failure). What the peak-end data show is
that what we anticipate with dread, and/or what we even experience at a given
time, can be worse than how we feel about it once it is over, particularly if
it turns out well or at least better than, or not as terrible as,
expected. And conversely, what we
happily look forward to and/or even enjoy in progress can be ruined
retroactively, not only by turning out badly, but by crushing our happy
expectations in addition. If you don’t
have expectations or desires for a particular result, not getting it won’t as
likely or as much retroactively ruin your pleasure during the experience. For example, consider a couple breaking up
after having good times together. This
is illustrated even better if those good time included sex they both
enjoyed. If one of them expected the relationship
to last and turn into lifelong marriage, but the other didn’t, then the breakup
before marriage, or divorce after it, can make one of them sorry s/he got
involved and emotionally invested, but leave the other with happy memories. The difference in such a case is not in their
experiences in progress but about their goals or purposes in
participating. The one just wanting a
good time, if that is truly all they wanted or expected, is still happy and
grateful to have had it. But the other,
who saw those good times as part of (or as a means to) something they thought
greater, more lasting, and more desirable can be understandably disappointed or
crushed. On one episode of Two and a Half
Men, a woman whom care-free Casanova, Charlie Harper has cheated on and/or
dumped after dating a while and with whom she has been cheating on her husband
with a lot, appears at his door distraught and irate, telling him off and
saying what a rotten cad he was, how he has made her miserable and ruined her
life, and how much she regrets having been with him, etc. When she leaves (without having shot him or
vandalized his home or car) his comment to his brother was something like “I
think that went rather well.” The
audience understood perfectly well his saying that, because Charlie only wanted
sex, not a relationship, and certainly not a commitment. So the end of the
relationship did not ruin anything really important to him, and the fact the
woman was upset was not of any real concern to him. But there is more to finding out about what patients want than just asking them, since they do not always know themselves or they can be mistaken about what they think they prefer or would prefer. Dr. Gawande does realize that: “doctors would sometimes have to go farther
than just interpreting people’s wishes in order to serve their needs
adequately. Wants are fickle. And everyone has … ‘second-order
desires’. We may wish, for instance, to
be less impulsive, more healthy, less controlled by primitive desires…, more
faithful to larger goals. Doctors who
listen to only the momentary, first-order desires may not be serving their
patients’ real wishes, after all.” (Gawande, p. 202) These points are all true, but there is much more to it than this. Wants are not only “fickle”, but they conflict in serious ways with each other even at a given time. One can desire to do something one fears to do and one can desire to do something one even knows is wrong or undesirable to do or that one will regret. It can be as simple as buying something fairly expensive one knows one will tire of before it is paid for or shortly thereafter. It is part of the human condition, long known, that we, often tragically, have conflicting desires, even conflicting first-order ones, sometimes with accompanying second-order conflicts as well. E.g., one can swear off ice cream to lose weight but crave some at the same time one craves not to be weak and give in to the craving or cheat on the diet (which I consider both to be first-order desires), while having the second-order desire to lose weight by not having the ice cream. In the Iliad Achilles has to choose between joining the military expedition against Troy, knowing that he will die a legendary, heroic death for a stupid cause and help win the Trojan War, or staying home safe and being “a tender of sheep” among women. He chooses to go with the military. But in the Odyssey, when he meets Odysseus in Hades, he then wishes dearly that he had chosen to remain home, a tender of sheep among women, than to be a hero in Hades among the dead. I presume that even knowing that, however, if he had to make the choice all over again, he would choose the same way he did, and then regret it afterward all over again. Surely soldiers with families to raise have the same sort of conflicting desires about going into harms way to protect their families on one level, but leave them vulnerable on another. The soldiers, for example, who died during WWII helped save their families from potential Nazi and Japanese tyranny and atrocities of the sort they had committed in Europe and Asia, but not from the bad consequences of a loss of a spouse, parent, or child. Moreover, choices don’t necessarily have to have all good or all bad consequences. Bad options can be mitigated in different ways. Bad consequences don’t have to have just deep valleys (i.e., ‘peak’ or significant bad moments] or even just terribly, miserable endings. First, and what should be easiest to know and to provide, whether a patient can be improved or cured or not, genuine, enlightened compassion can go a long way to ameliorate or prevent emotional and psychological suffering, including fear. Coping is not just about trying to be cured. And trying to help people cope is not just about trying to cure them or improve their physical conditions or abilities. It is about having and showing sincere caring and seeing the patient as a fellow human being. In the 1991 film The Doctor, starring William Hurt as a physician diagnosed with cancer, there was one particularly emotionally strong scene for me, where he had to walk alone down a long corridor to one of the labs for radiation or chemo or some diagnostic procedure (I forget the exact details), but the way it was filmed made it seem lonely, terrifying, and dismal in a way that would have been easily mitigated by someone’s going with him who understood his situation, even if a hospital aide of some sort simply assigned to go with people during that otherwise lonely walk. Sometimes a companion, even if (or especially if) a stranger can be important. I tore my Achilles tendon while playing tennis, but it never hurt, and I still had some motion in my foot, though very little and I basically just picked up the foot and then planted it stiff-legged to walk on it. I asked my orthopedic surgeon who said it was torn and should be repaired tomorrow (before it contracted and curled up and would be hard to stretch back into position to reattach) why I could still move my foot up and down if it was torn. He said he didn’t know but he was pretty sure it was torn. His honesty in admitting he didn’t fully understand it made me trust him. I was particularly concerned that surgery would prohibit me from photographing the four weddings I had scheduled to photograph within six weeks, the first in five days, which I thought I could do limping along in the condition I was in now, and he assured me surgery would not prevent me from shooting the weddings. He was correct, but it took a lot more effort than he led me to believe it would, including using a wheelchair to get around and crutches while standing to shoot the pictures from the right height. After the surgery during follow up visits we talked about things other than medicine, and I found him very interesting and exceptionally understanding and compassionate. A few years later, that led to a fun doctor-patient moment. I one day developed tenderness in the other Achilles. I wondered if there was such a thing as Achilles tendonitis and looked it up on Yahoo (the main search engine at that time). It said there was, and the signs and symptoms listed matched mine, and it said that it should be seen by an orthopedic doctor to prevent it from rupturing. When I went in to see him, I said I wanted to guess the diagnosis first before telling him my symptoms. He was amused and went along with a little chuckle. I told him I thought it was Achilles tendonitis and had looked it up “on the Internet” (which was just a novelty to most people at that time) and that it had said there was such a thing. He asked what it said about it and I told him the signs they listed and also the part about seeing an orthopedist to prevent it from rupturing. He found the idea of this information being on the Internet, and me finding it and putting so much stock in it, amusing, and he said: “It is Achilles tendonitis. But I have never seen, heard, or read about it causing a rupture, so I’ll tell you what – we could not treat it and see whether ‘the Internet’ is right.” And he had this great wry smile. I told him I would defer to his wisdom rather than the Internet. He gave me a boot to wear for it, strongly recommended ibuprofen, which I took though I hate to take anything and see it as a sign of weakness or potential beginning of a road to dependency, which he knew how I felt because I never used the morphine drip after my previous surgery (and thus, this time, suggested strongly), and the soreness of the tendonitis was gone the next day. (My maternal grandfather, at whose house I stayed almost every day growing up had become addicted to Demerol after surgery that left him an invalid before I was born, and it was terrible watching him be so dependent on getting his shots of it to prevent terrible, agonizing physical pain he otherwise experienced. That and all the other adverse potential side effects of drugs makes me averse to taking them generally.) Another physician was humorous in a different way. When I was in my mid 30’s, one day I noticed some sorts of bumps on my skin in my pubic area; they were small, round, and smoot and sort of plastic looking. They seemed to be possibly increasing or spreading. I thought they might be some sort of warts. One was on or near the base of my penis. My across the street neighbor was a nurse, and I asked her if it would be okay for her to look, because I was worried I had venereal warts. She looked and said that although she didn’t know what they were, she knew they were not venereal warts and that if I had venereal warts, I would know it because venereal warts were bad. She asked why I thought they might be venereal warts and I said “Because they seem to be some sort of warts and are on ‘my veneer’, as it were – the place where one gets venereal diseases.” I don’t like going to doctors without some sort of clue what to expect and to be able to evaluate their diagnoses or treatments, and since I remembered reading something about warts on babies in Dr. Spock’s Baby and Child Care I looked it up in the book. The description that seemed closest to what I was seeing was what he called “contagion warts”, so I called to schedule an exam with a nearby dermatologist I found, and when the nurse scheduled the appointment I asked what the treatment would be for contagion warts if that turned out to be what I had. She said application of liquid nitrogen was safe and easy and should work effectively. I went in and the dermatologist was an older woman from Paraguay, perfectly fluent in English, but with a bit of an accent that made her seem smart and exotic. She told me the medical term for what I had, and I asked if that was also known as “contagion warts”. She said it was, and asked “How you know contagion warts?” I said, “Dr. Spock.” She said she didn’t know him; was he my internist? I tried to explain who he was, but she really wasn’t interested in that. She asked if I knew the treatment, and I said, “liquid nitrogen to freeze them.” “How you know that?!” I said her nurse had told me when I made the appointment and asked about it. After she sprayed on the nitrogen, she pointed to the latest outbreak of spots on my skin and said, “Do you know what that is?” And I said, “tinea versicolor”. “How you know that?!” I said, “I was first diagnosed with it when I was a teenager and have periodic recurrences of it, but I don’t treat it because that requires using a sulfur compound that stinks too much.” She then smiled and said “Hah!! Finally something you not know!! There is new treatment now that does not smell, and is better!” So she prescribed an antifungal cream that worked really well. She was a hoot, and that was a fun visit. Of course, it was also a curable condition, which didn’t hurt the matter. But she would be the kind of dermatologist I would want for something serious or even life-threatening. Later I found out she also was interested in learning photography and studying literature, two things I taught informally, but she was not interested in the specific fields of them I could teach her about. Still, she was the kind of doctor I could feel good about being treated by, someone with a sense of the human spirit, someone not just a technician. Humor and compassion of the right sort serve not only in their own right, but as forms of distraction from undesirable elements of a physical exam or (discussion of) treatment. When I was fourteen I was diagnosed with an anal fissure that sometimes would bleed. When the bleeding would sometimes recur, once every year or two or three at that time in my life, I went to a proctologist, and that was always scary and embarrassing. After leaving grad school and moving to Birmingham, the proctologist I found one year asked me about my work and other facets of my life, in part to determine what might be stressing me in case stress played a role. He asked about recreation and I told him I was teaching myself to play the violin, and it turned out that he was a violinist who loved to talk about playing and took an interest in how well I was doing. I saw him as a patient maybe three or four times in the next five or six years before he retired, and during each visit he made sure to give me verbal pointers about playing the violin after he did the exam. That, coupled with his not finding any serious problem (especially coupled with his not finding any serious problem), made the appointments be actually enjoyable and memorable experiences in ways none of the other proctoscopic exams with other doctors were, even though they were equally medically uneventful – except for the guy I went to once who took a brief look after rushing back to his office late from lunch, said I needed surgery as soon as I could schedule six weeks bed rest (which was pretty much never), and handed me a pamphlet about the surgery. While he scared me, I felt he must be looking to buy a bigger boat and wanted me to contribute to it through Blue Cross. I never went back to him, but the next gastroenterologist – the chairman of a university gastroenterology department -- I saw a few years later said he never heard of the condition the guy said I needed surgery for and that I didn’t need any surgery. (I suppose, of course, perhaps it healed itself….). The right kind of humor in scary and/or embarrassing situations can also help. As part of a routine physical for my age at the time during a subsequent appointment, that later gastroenterologist set me up for a routine barium enema – a procedure definitely not devoid of discomfort, anxiety, or embarrassment. When I arrived for the procedure, I was greeted by a female tech who would assist the person doing it, and who explained the procedure to me and what to expect. She then exaggeratedly adjusted one of her rubber gloves with a loud snap as she said with a smile and a twinkle while looking right into my eyes: “For the next half hour, I am going to be your best and most intimate friend.” That not only allayed my fears and embarrassment but made me laugh and feel comfortable and believe that this might be a far less dreadful experience than I was anticipating. She clearly understood my anxiety and embarrassment but also intuitively correctly sensed she could use that kind of humor with me to ameliorate it. I suspect that humor works by 1) showing that one understands and sympathizes with the fear or sadness you must be feeling without magnifying it by mentioning or dwelling on it and at the same time 2) showing one wants to lessen or remove those emotions, in part by distraction and in part by turning the cause of it into something that is funny, particularly in a clever, subtle, perhaps even absurd but logically connected, way in order to override them. The idea is to use the same ingredients that are troubling you to make you laugh by transforming and transcending the situation. Of course one can do it poorly or fail with any particular person one misreads, or one can overstep. I was photographing one particular wedding where the couple getting married were in their late 30’s, and the groom was the youngest of numerous siblings. His father had been married three times, and his current wife was there along with both former wives, one of whom was the groom’s mother and the other a step mother who was close to him too. Prior to the wedding, the father was joking and teasing me and his son, and was relaxed and having a good time. But after the ceremony when I was trying to shoot the family picture (a large group), the father just would not smile, and nothing I said to elicit a smile from him was working. He finally asked why I was picking on him, and I said so that everyone could hear: “Because you are not smiling, and it shows up clearly in the group in contrast to everyone else, and will ruin the picture and make both you and me look bad. And I just don’t get it, because I would have thought that being under the same roof at the same time with all the women you have ever been married to would have made you really happy.” That brought a huge laugh out of the group, and when it subsided he asked where my car was parked. By then I had already decided I had probably overstepped, and I said “If you only hurt my car, that will be okay.” And then he smiled nicely in the rest of the pictures. During the reception he came up to me and put his arm around my shoulder affectionately, saying “You hit the nail on the head about what was bothering me, and the way you did it let me get over it and relax. Thank you.” Basically, compassion, even mixed with dark humor in a dire situation can go a long way for a patient. When my brother-in-law was diagnosed with a slow, but likely terminal blood condition, the doctor who made and told him the diagnosis was also his best friend. My brother-in-law had always been something of a ‘grumpy old man’ with a very dry, usually cynical, acerbic, pessimistic wit that often pointed out negative qualities in people and situations in a wry way, and his friend, after giving him the diagnosis and prognosis, said, “Now there are support groups for people with this condition, but you should not go to any of them, because you will bring all those people down.” My brother-in-law relished telling that story, though probably not sufficiently to make having the condition worthwhile. Patients and friends can do this for each other too. It doesn’t have to be doctors or nurses. When I was waiting in the X-ray lobby for my turn, there were lots of men my age there with me who seemed to have some sort of injury or other. I asked them what their wives said when they got injured, and pretty much to a man, their wives blamed them for trying to act young or doing something foolish they shouldn’t have been doing. That tended to make them feel worse, until they found they were all in the same boat that way or apparently were all married to the same woman. I know finding it out made me feel better. In college, my roommate’s fiancé had an emergency appendectomy and when I went to visit her in the hospital, she was in a large ward with dozens of other patients. One of them was hesitantly calling for a nurse, but no nurse was around at that moment. I went over and asked her if there was something she needed that I could do or if she needed me to track down a nurse. She said ‘no’ and that it was okay. An older lady in another bed near her motioned to me and whispered in my ear that the girl’s legs were paralyzed and that her bedpan was full and needed to be emptied. I asked her where I could empty it and she pointed me to the facility at the side of the ward. I took the bedpan to empty it and rinse it out. The girl was embarrassed. She was sixteen and, otherwise in the peak of health had suddenly a few days ago become paralyzed, and no one knew what it was. She had come from out of state to the University Hospital here. Having some stranger, particularly a college boy, empty her bedpan was the height of embarrassment to her, along with her embarrassment and concern at being helpless and in this setting. She was mortified when I came back and thanked me but also sort of wished I hadn’t done it. She was grateful and regretful at the same time. I just laughed and said “Oh, that’s okay. I know you would have done the same for me.” That made her laugh because she knew that I knew that no, she wouldn’t have. So we got to talking and I found out that she fully intended to walk out of the hospital on her own at some point, and I said that I would like to escort her when she did. Everyone else feared the worst for her, but she didn’t want to hear or think that at the time. I felt that encouragement in the face of lack of anyone’s knowledge to the contrary at that point couldn’t hurt. There could be time to come to grips with bad news later if necessary. At that point it was not necessary and would have just been unnecessarily discouraging to her. When it was time for me to go, as I got part way across the room, she asked if I would come back to see her tomorrow, and I called back “Of course, I will, so don’t go running off with some other guy before then.” There was an audible unison gasp in the room among the other patients who thought that was a terrible gaffe or indelicate thing to say given her condition, but the girl laughed and lit up with a huge smile and ‘promised’ she wouldn’t run off with anyone. I don’t know whether they were ever able to diagnose her at the time, but she probably had Guillain-Barré syndrome, which righted itself within a week or ten days, and I was able to escort her out of the hospital after convincing the staff to break the rule to wheel her across the threshold, and let her take that last step out the door on her own with my support if necessary, because it meant a lot to her to be able to walk out as she had vowed to do. The last that I spoke by phone with her mother many years later, the girl’s health had remained perfect with no signs of the paralysis, and she was now married and had children of her own. But unbridled rosiness is not always appropriate. At my apartment complex one time, a seven- or eight-year-old girl accidentally slipped going down some concrete steps and scraped the back of her leg to where it was bleeding. One of the neighbors brought out some bandages and another had some iodine. The girl was afraid their applying it was going to hurt, and one of the women said it wouldn’t. Well, yes, it would, and then credibility was going to be out the window. So I said before the iodine was applied that “Yes, it will hurt a bit, but only for a short time, and it would help prevent an infection that would hurt more.” That calmed the girl down and she didn’t cry at all when the iodine was used. Of course, sometimes you can say or do the wrong thing. I thought I was really good with little kids, and when a neighbor was going to be out of town on business when his wife had to take their three-year-old daughter to have the child’s blood drawn for an upcoming surgery, I volunteered to meet them at the hospital to help out. The girl seriously resisted the tech, until I suggested letting the tech show her on me how the procedure worked and that it was no problem. So the little girl watched as the tech drew blood from me – and then she totally freaked out so bad that they just about had to pull her off the ceiling and hold her down while they drew the blood. Apparently I had lost my charm with kids. And I am sure that some people would probably not like having a barium enema technician snap their glove and say they were about to become your best friend for a half hour. But if you can at all ‘read’ the patient correctly, humor can be a great help showing compassion and wanting and working to alleviate it in a scary or even very sad situation. But besides just being compassionate or genuinely showing sympathy or empathy (with or without humor), it is also important to help a patient see and interpret their experience in a more positive way, or for a patient to be able to do that on their own. And it is also important to cast a treatment or even a condition, in a light that makes it reasonably appear more desirable or tolerable than it otherwise would be. My father had, as a youth been a pretty good amateur baseball and basketball player and had always had great hand-eye coordination. When he was 83, he was visiting my sister’s family 500 miles from home, when he fell while outside kicking a soccer ball back and forth in the yard with his young grandson. He had never played soccer as a kid. He fell because when he went to kick the ball on one pass, he accidentally got his foot on top of the ball instead of into it, and he lost balance. He hurt his shoulder when he hit the ground. He told the grandson not to tell his mother that he had fallen. He was embarrassed that he had been “clumsy” and guilty of doing something stupidly risky for his age, which was how he saw it. The next morning, he could not raise his arm above his waist. He made up some flimsy excuse about arthritis flaring up and told his daughter that he had better drive back home before it got worse. He drove himself the five hundred miles, basically with his left hand, which is not his dominant one. After he arrived home he saw his physician who determined it was probably a partial tear of the rotator cuff, that rehabilitation and time could alleviate sufficiently, with surgery being unnecessarily risky at his age, and who put his arm in a sling. That did not make him feel any better about himself or his injury because, although the sling helped prevent more pain, it just even more embarrassingly called attention to his perceived clumsiness and poor judgment of activity to have done with his grandson. Except for grocery shopping, he would not go out, and he avoided all his friends and acquaintances. He did not go to the synagogue where for a number of years, since his retirement he had gone daily to help there be a required quorum to permit the morning service for those in mourning. He was ashamed about the cause of his injury and the limitations it caused him. He could not shake hands with anyone or do some of the normal things, such as reading a book, that generally take two hands. He never told my sister about any of this, and his grandson had kept quiet as he had been told. Unaware of all this, I called from an equally distant city where I lived to inquire about his trip and to engage in general conversation. I sensed there was something wrong, and with prodding he confessed what had happened and how he was taking it. Just commiserating with him and saying his friends would understand, etc. didn’t work, and I felt that he was in a downward emotional spiral that would not be good for him. So even though I knew he normally was not prone to be philosophical or to find humor in troublesome situations, I took a chance anyway and said “Why are you embarrassed about it?! You should be proud of it! There aren’t many 83-year-olds that sustain soccer injuries!” Fortunately, that actually made him laugh, and he saw it as a good perspective to have. I added that “it is just like your mom always used to tell you and your brothers whenever you got hurt as children: ‘it’s all in growing up.’” He liked that too. After that, he resumed his normal activities and told with great pride and glee why he had to wear the sling – that he had got hurt last week playing soccer. I was actually surprised that it worked, and there are some people much less flexible about interpreting their conditions favorably and certainly not in finding humor in them. But when it works, it is a good thing. My wife’s grandfather had, in his later years, developed what was then called senility, and now called dementia. But he lived in the house he had lived in all his adult life and he could get around town by walking, even going to the grocery store on his own, cutting some backway that took him over railroad tracks and was a shortcut. I went with him one time, and it was good he knew the way back because I would never have remembered it. Yet he normally couldn’t recognize family members he didn’t see every day; and he didn’t remember much news or other sorts of things that were recent. But he took it all in stride, found new delight in meeting people he didn’t remember were old friends or family members, showed great wit, even about his condition, and just went along having a good time despite the dementia. When we took our first baby to Pennsylvania to meet him when she was six weeks old he held her in his arms and said “Darling, when you grow up you won’t remember me. But that is okay, … because next week I won’t remember you.” And he had the biggest grin on his face and best twinkle in his eyes when he said it. One day sitting on the porch with him as we talked, his eyes followed some older teenage girls walking by on the sidewalk. He was wearing a light sweater on the porch, and they were wearing short shorts and halter tops. He was not unappreciative. He looked back at me and knew I had seen them too, and just said with a smile again, “I guess it must just be a lot warmer out there on the sidewalk than it is here on the porch.” He had little, virtually no, short term memory, but he made the most of each moment as he lived it and as he anticipated others with joy. Many years later, when his son, my father-in-law developed similar dementia, my father-in-law did not adapt to it like his father had. He was mostly frustrated and angry. My mother-in-law had been an anchor for him, but after she died fairly soon after being diagnosed with advanced cancer, he was pretty much lost without her. He was still strong as an ox, and was strong-willed about wanting to do things that he couldn’t safely do, such as drive or even go for walks because the past he could remember was not from neighborhoods he had lived in in the most recent thirty years. He would rattle around our house looking for his wife and wondering why he was with us, etc. and constantly wanting to go home, though he didn’t know where home was. He could not enjoy anything on television, even sports that he had dearly loved, because he couldn’t remember what he was watching and how what was going on followed from what had happened earlier. He asked the same questions over and over and over, and was disappointed, frustrated, saddened, or upset about the answers each time. He didn’t understand or remember that his memory was bad, in the way his father had realized about his own memory. His father didn’t ask about much, probably because he realized he may have already asked it and wouldn’t remember the answer anyway. One time when I was with his father in Florida for a family vacation there, he saw pine trees as we drove around and asked if we were in Canada (where he had once lived a little while as a young man) and when I said it was Florida, he said that was nice too and was satisfied the rest of the time. He enjoyed the beach and when a flock of pelicans flew over while we were talking he said correctly that there were nine of them without missing a beat. He was satisfied living in the distant past and in the immediate present, but my father-in-law, when he became like that, wasn’t. Apart from the fact that the older man lived in the same town that had not changed much most of his adult life, so that he could navigate to and from his home by distant memories, it was not clear why he adjusted to his dementia much better than his son did, who never really came to grips with his own condition. The older man had severe short term memory loss but he didn’t suffer from it, didn’t sorrow or anger over it. My own father lived to be 95 and suffered some short-term memory loss in the later years, deciding, with prompting from my sister, to move into an assisted living place he had visited friends in and that he liked well enough. He one day told me on the phone that he was worried that his mind was starting to go and I reassured him that he was as sharp as he ever was. He said that was good then, and I said “No, not really.” And he got it, and laughed at that. He also laughed when he said he worried about forgetting things, and I asked, “Like what?” and when he could name them, I would say he hadn’t forgot them, and when he couldn’t remember what he had forgot, I would say “then don’t worry about it; just forget about it. Oh wait, you already have.” But I was serious that despite some short-term memory loss and some repetition during phone calls, he really was not deteriorating or losing his mind or faculties. He was able to function quite well and didn’t really seem that much different otherwise. A different perspective does not have to involve humor. When my mother was thought to be on her deathbed in the hospital my father called me that morning to drive up, but didn’t think I would get there in time. It was a ten-hour drive. I shaved an hour off that, but it turned out she had rallied a bit in the meantime anyway. When I got there, she was conscious and coherent, and I had thought about what to say to her if she was. Whenever anyone died, she would always preface the news by asking if we remembered the person, which had always struck me as odd, especially if we had been with them recently. But I realized she meant that we should always try to remember them and that was important to her. So when I arrived at her bedside, I assured her that I loved her and would always remember her, and she was moved by that. She then wanted to talk and also wanted some soup but was having difficulty using the spoon. I took the spoon and was going to feed her. She did not like feeling helpless or being waited on and she was embarrassed. I said “Look, you used to feed me all the time and didn’t mind doing it – even sometimes enjoyed it. So I am just returning the favor.” She liked that idea and let me feed her. She ended up living for another week. I produced the two pictures of the wheelchair with the Mercedes in this endnote[ii] because it struck me as odd that two different vehicles for transportation evoke such totally different emotional responses in those who observe them. And one time when I photographed a family at a local botanical garden, the grandmother disdained the use of the garden’s free wheelchair even though the walk to the spot we were doing the picture was slow and difficult for her. I asked her whether she would feel the same way if the wheelchair was made by Mercedes, and she said, no; if it were, she would happily use it. I wrote Mercedes to recommend they get into the wheelchair business in part as a public service to change perception of the disabled who use chairs, but …. One final story about perspective: I injured a knee my freshman year in college, and had a follow-up visit with the orthopedist his office in the university health building on the second floor. I was still on crutches and the knee was still painful to flex and straighten. As I started down the steps to the ground floor, I momentarily forgot you need to keep the crutches lower than your feet when using stairs, and I stepped onto the top step first, which I immediately realized was going to make me fall down the steps because I was caught in the air for a second just balanced on the two crutches and couldn’t reach the ground as my body was going forward. The idea of falling on that knee down the steps terrified me, and the terribly stupid idea immediately occurred to me to jump and hurdle all the twelve or so steps in that flight to the landing below that was at a right angle to the next set of steps. So I catapulted my body forward hard enough to go airborne and clear those steps. In flight, the idea didn’t seem as good as it first had, but I ‘stuck the landing’ perfectly on my good leg and the two crutches, and I turned my body as I landed so that I could stop my momentum against the landing wall with my shoulder. I had made it safely. I was totally embarrassed at being so stupid as to begin the fall in the first place and then to have made the foolish jump, and I looked around to see who had seen it. I was grateful no one had. I was the only person in the area. But then I was immediately disappointed no one had seen how cool it was. The human mind is apparently capable of both embarrassment and pride at the same time for the same act, depending on the light or angle from which it is viewed. Perspective is important in how we see and think about things. But more important than compassion, empathy, perspective, and humor is an understanding of what makes life (and what makes any difficult medical treatment) worthwhile, particularly in the face of end-of-life circumstances such as terminal illness or progressive debilitating injury. Both Dr. Kalanithi and Dr. Gawande mention the concept of treatment’s being worthwhile, but it needs to be developed much further because understanding it more fully is crucial to helping patients make the best decision and have the best perspective about their conditions. Where they do write about it, they say: V’s surgery, chemotherapy, and radiation treatments were trying, but a success. He was back at work a year later, just as I was returning to my clinical duties in the hospital. His hair had thinned and whitened, and the spark in his eyes had dulled. During our final weekly chat, he turned to me and said, “You know, today is the first day it all seems worth it. I mean, obviously, I would’ve gone through anything for my kids, but today is the first day that all the suffering seems worth it.” How little do doctors understand the hells through which we put patients. (Kalanithi, pp. 101-102) Doctors in highly charged fields met patients at inflected moments, the most authentic moments, where life and identity were under threat; their duty included learning what made that particular patient’s life worth living, and planning to save those things if possible – or to allow the peace of death if not. (Kalanithi, p. 113) In 1908, a Harvard philosopher named Josiah Royce wrote a book with the title The Philosophy of Loyalty. Royce was not concerned with the trials of aging. But he was concerned with a puzzle that is fundamental to anyone contemplating his or her mortality. Royce wanted to understand why simply existing—why being merely housed and fed and safe and alive—seems empty and meaningless to us. What more is it that we need in order to feel that life is worthwhile? The answer, he believed, is that we all seek a cause beyond ourselves. This was, to him, an intrinsic human need. The cause could be large (family, country, principle) or small (a building project, the care of a pet). The important thing was that, in ascribing value to the cause and seeing it as worth making sacrifices for, we give our lives meaning. (Gawande, pp. 125-126) We do not want to endure long pain and short pleasure. Yet certain pleasures can make enduring suffering worthwhile. [emphasis mine. Garlikov] The peaks are important, and so is the ending. (Gawande, p. 239) When he was in the grip of it, the pain became his entire world. He tinkered constantly with his doses, trying to find the combination that would let him feel neither pain nor fogginess—feel normal, like the person he’d been before his body began failing him. But no matter what the drug or dose, normal was out of reach. Good enough, however, could be found. … Each day, he found moments worth living for. (Gawande, p. 250) Drs. Gawande and Kalanithi hold that an important role of the physician is to help people have the treatments that allow them to have their best days possible according to what the patient deems is best for them. I believe that is partly right but only if what the patient thinks is best is most reasonable for him or her and most consistent with his or her reflective views about what they really want. Determining that requires bringing to light, and keeping in mind, many of the complexities involved in making choices about what we think is best. I want to examine what is involved in that, not only in end of life or terminal and progressively debilitating illnesses and injuries but also in normal, healthy daily living. End of life cases can be considered to be the application of general decision-making principles under special circumstances where there are fewer good options, most of the bad ones are worse and worse, and there is less and less time to bring worthy pursuits and goals to fruition. In end of life cases, or in any other cases that involve the most dire and dreadful circumstances, it must also be asked whether the best life possible or the best day possible is good enough to make life worth living, or good enough to choose a particular action or treatment option or to reject or discontinue treatment. But that is not quite the right way to consider the question. What is really at issue is not what makes life worth living, but what makes enduring any suffering in life worthwhile. But this is not just about peaks or valleys and endings, and it is not just relevant only in devastating disabilities or terminal illnesses. It applies throughout the whole of life. It just becomes most noticeable as a problem or dilemma in end of life types of cases. Except for people who are particularly plagued, distressed, or depressed by what most people consider normal disappointments, bad news, sad events, and troublesome problems in life, choosing the best course of action on a daily basis doesn’t consider death (particularly suicide) to be one of them. The presumption is to consider life a good, and normally that is the reasonable presumption, so the normal question is not whether to choose to live or to die, but which choices likely yield the best way to live. I want to examine both questions because they shed light on each other, and because in end of life cases involving progressive, debilitating, terminal circumstances both considerations frequently arise, often together. In the previous passage from Being Mortal, Dr. Gawande points out that his father could often find a way to treat himself medically that, “though normal” health was out of reach, “good enough ... could be found.” The question usually arises though, sooner for some and later for others, what constitutes “good enough” and what to do when nothing helps one have a day that is “good enough”. We mistakenly tend to think of quality of life in terms of the relative duration and intensity of joys versus the duration and intensity of sorrow and suffering, where the quality of life is better the greater the balance of joys are to sorrows. But what that misses is that most lives do not have a higher balance of joys than sorrows or sufferings. Dr. Gawande points out that “In the end, people don’t view their life as merely the average of all of its moments—which, after all, is mostly nothing much plus some sleep.” (Gawande, p. 238). However, the “mostly nothing plus some sleep” is not accurate at all. For most people, if we consider just duration and intensity of joys versus duration and intensity of suffering and sorrows, although it is true we don’t usually remember it that way, we do experience much more suffering and sorrow than joy, in part because suffering and sorrow tend to be more intense and also spiral or magnify themselves in ways that joy and happiness do not. Also, I would count as at least slightly negative the time we spend working (at most jobs, unless you really love your work), waiting, traveling from one place to another just as a means to getting there, not as an adventure in itself. We spend a lot of time just ‘killing time’ or occupying it with chores or distractions between more important moments. Much time is spent in work and, for students in study, or in at least minor drudgery we only do as a means to some desired end. Much of life is literally and figuratively spent in rush hour on the freeway, often to a destination that is at best a stop on the route to where we really would prefer to be. And much is repetitive and more necessary than satisfying. We do the same dishes every day, the same laundry every week, the same yard work all summer every year, the same kind of job each day, hear the same kind of news, and basically spend much of our time like Sisyphus, pushing a large rock up a hill, which, once at the top, it will roll back down to be pushed up again. 18th century philosopher David Hume put it in the strongest, bleakest way in his Dialogues Concerning Natural Religion (i.e., evidence about God from nature, not from historical revelation), and although life is healthier and longer for most people now, most of what he wrote is still true and worth considering, not only for what it articulates so well, but also for what it misses seeing. For as observant and understanding as Hume usually was, he lost sight of what makes life worth enduring all the suffering. It is something besides the amount and intensity of sorrows and joys, and I will get to that after this excerpt from Hume (1779):
Of equal or greater importance than duration and intensity is the significance of the joys and of suffering and sorrow to the person or patient. Very few, if any, people have lives which have more joy than sorrow or languor, forced wasted time, and weariness as we work and simply often just wait in moving from one eventful moment to the next. But it is significant events and perceptions that are important and memorable to us, and the good ones somehow make up for a lot of the bad moments, often even the significantly bad ones. That is why the past seems to move much faster than the future: the highlight reel of our memories is always faster than the play by play of the game. Memory edits out the wait and prep times and the other insignificant moments life has to experience and endure at the time. But it doesn’t just do it in terms of peaks and ends; many memories or highlights are just interesting to us or memorable in some way like the math/logic problems I pointed out are for some people. Others are significant for some reason though not especially joyous or sad. They are not in any normal sense of the words “peaks” or “valleys” of joy in either intensity or duration. For example, when my children were born, I was present in the delivery room, and kept expecting that ‘bonding moment’ you always hear about from fathers who claim it was a highlight of their life (but who seem otherwise likely to have had no interaction with their children until the children were old enough to play sports or some such), but it didn’t happen. I was grateful both children were born healthy (according to their APGAR scores by the nurses, but not according to their appearance, which seemed something akin to having been run over by a truck), but was more conscious of a sense of responsibility for their future well-being. Actress Olivia Wilde, when asked about her parenting philosophy, said about her infant child something like “Right now I am just trying to keep her alive.” That is a responsibility in itself, let alone helping them learn and grow to be independent, successful, content with their own lives as they go through each different stage of development and each day in it. And it is a responsibility that often takes constant effort in the modern world with its many added dangers to the natural ones for children, whether having to guard them against being hit by a car in a parking lot or being left in a hot car in a rearward facing car seat in the backseat of your car because they fell asleep during a trip you don’t usually make with them and forgot you had them as you were concentrating on getting to where you had to be. But when all goes well, we forget about those efforts and the time they take, because though they are important to remember to do, they are not important nor interesting to remember having done. Being careful to watch where you are driving does not make you remember what you just saw once safely past it. Careful attention to the present or near future does not necessarily embed experiencing them in long term memory. Another one of my fond memories which sometimes comes to mind, is of an experience that occurred during a few days I spent in the infirmary at college. Most of the nurses would just tell you to wake up in the morning so they could change the bedclothes and do whatever they needed to in order to have you and the room ready for the doctor’s rounds. But there was one older nurse who woke me up by stroking my back through the covers for just a few seconds. It was a simply pleasant way to be awakened, particularly contrasted with just being sharply told to wake up and get out of the bed. The duration and intensity of the pleasure were not that great, but it was nevertheless significant and meaningful. When I was a child, my father bowled in a league on Sunday mornings, and he would take me with him to the bowling alley. It was a really boring time for me for the most part, but it was made worthwhile (or almost worthwhile) by his letting me lie down on the bench while he scratched my back during their warm-up practice time. After that I was left on my own elsewhere in the bowling alley and not allowed to be on the bench to disturb his team’s match. Now, I do consider having my back scratched one of the greatest kinds of pleasures to have, but it was only a few minutes of backscratching compared with a few hours of boredom later, and having my back scratched does not provide what might be considered an intense kind of joy. But it is most pleasant. On the occasion later in life when I had my Achilles tendon repair and woke up in my hospital room after surgery, it didn’t hurt that my nurse turned out to be a former student of mine whom I had helped sort out a couple of personal problems when she was in my course. Again, it was not that it was a great joy or some sort of pleasure that lasted a certain amount of time, but it was meaningful. Even when a joy is intense, it may be something minor in duration and minor in any kind of ‘objective’ importance in the great scheme of things, though important at the time to the person experiencing it. Probably one of the most exciting moments in my life was the first time I was finally able to ride a two-wheel bike after months and months of trying unsuccessfully to do it. Two of my friends helped me learn by holding the bike up from each side until I could balance. When I finally could get on the bike myself and start it and ride, it was a total thrill. I still enjoy riding a bicycle, nearly seventy years later, but that initial ride by myself was really exciting. Or one time, the willingness of an older stranger to listen sympathetically and offer encouragement on a train ride home during a trip on which a girlfriend broke up with me when I arrived at her college from mine, which she could have spared me the trouble of making by just telling me over the phone. Or the most encouraging comment to a friend of mine and me, by an old chemistry professor we happened to meet, after we had just found out we did unexpectedly poorly on our first freshmen chemistry exams and mistakenly thought that meant curtains for our pre-med studies and hopes. Or the early morning walk to work one day, alone on the sidewalk when a Volkswagen Beetle approached going in the opposite direction and the female driver slowed down to check me out as I was peering in to her car to check her out – each of us realizing immediately what we were both doing and then smiling, laughing, and giving a wave before we each kept going. Not a long experience, not an intense experience, but a happy and memorable one just because it was cool and ‘human’. What makes our lives worth living and/or better living one way than another is not necessarily the quantity or proportion of good experiences to bad ones, though a higher proportion of good to bad is generally better (all else being equal). Nor is it the quality or value and intensity of any particular good experience, nor its duration. It is simply whether our experiences and the hopes for, and anticipation of, likely future ones make our lives, in even some small way, worth continuing through the adversity and suffering we will have to endure to achieve them. It is about finding worthwhile significance in our experiences, no matter how little time or physical ability we have remaining, no matter how limited our material resources, and no matter how much our pain or suffering. If there were not pain, suffering, and sorrow, the answer to what makes life worth living would be just to experience what good it has and joy it brings, and the more, the better. Now, with regard to diagnosis of terminal illness or progressive injury, most people hope for a cure or remedy. But that is only in terms of extending life somewhat longer, not about making it permanent. It is not about the hope of immortal survival – none of us is going to permanently stave off physical death of our life on earth; it is about whether in whatever time we have left, something can be worthwhile or something can be expected or anticipated or hoped for that is worthwhile, particularly what is most worthwhile under the circumstances. Many think that treatment in cases of terminal illness is about keeping people alive in hopes a cure will be found; but there are far better reasons to keep people alive, because there are other things they are more likely to achieve than a cure – things they care deeply about or could if they were helped to find them. In other words the point of extending life, whether for long or short, is to allow people time to achieve what they reasonably consider to be benefits they desire to experience or obtain (and that make enduring any suffering or sorrow worthwhile to have). Since there is no vaccine for death and no permanent cure for mortality, the most we can hope for is the ability to do what is important to us in whatever time we have left. Normally, that will be different things within different ranges of time, but even the shortest times can allow significant and worthwhile good. The Hume passage misses all this. Hume pointed out all the evils and
unpleasantries in the world, of which there are many. But what Hume lost sight of was the joys,
whether a joy of discovery of some insight, a joy of accomplishment, a joy of
intimacy or love, a joy of friendship or of a small but unexpected kindness
from a stranger that manifests a connection of humanity, a joy of family, a joy
of beauty in art or nature, a pleasant surprise, the joy of being “in the zone”
of trying to accomplish something or solve some problem or figuring out
something (even in many cases when one fails to accomplish the objective or
solve the problem, for there can be the joy of being ‘lost in the attempt – of
getting outside of one’s self and one’s normal cares – and the joy of
‘stretching’ one’s self). Aristotle said
that happiness is an activity of the soul in conformity with excellence, but I
would add “and/or in the pursuit of excellence.” I encourage my philosophy students to discuss the questions they have to answer each week with their family, friends, and work colleagues. Many do. The questions are difficult but potentially intellectually stimulating, and I try to cast them in challenging, odd or unusual ways to make them fun and memorable. It tends to go better with work colleagues than with family or friends, who tire quickly of being mistaken in their initial attempts to give what they think is the obvious answers. But some of my students had a joy in even the frustration of trying to figure these things out – though their families did not share that joy. The fact that they thought about this so much, frustrating as it might be, gave them a certain amount of excitement as they tried to think up some way to answer it. I myself find a stimulating intellectual challenge to be one of the most worthwhile things in life that makes me feel alive, and I would say between that and the pursuit or attainment of emotional intimacy (which does not necessarily require physical proximity, and does not necessarily occur with either physical proximity or even sex), those things make my life worthwhile, and best, to me. When I have solved a problem I have been working on, that is at first exciting, but then it becomes something akin to finishing reading a good book and being glad to have read it, but sorry it is done. I even get somewhat depressed sometimes after that eureka moment, when I am done savoring it, and realize now I don’t have something else to work on to occupy and excite my mind in that way. Other people may like other things, such as tailgating at football games with friends, teaching or just enjoying time with, their grandchildren, traveling, playing golf, doing photography, or just relaxing and taking it easy, preferably in a comfortable and scenic environment. Some people even look forward to and enjoy playing golf, which is a triumph of hope over experience, illustrating my main point, since a few good shots here and there make enduring all the bad ones worthwhile and give hope there will be more good shots in the future. . ;-) (I grew up caddying, so golf to me is like a lot of hard work; and since I vastly prefer tennis, golf courses, to me – other than being the most beautiful places in most cities to take pictures or to walk, particularly at sunset – are just large wasted spaces that could have been used for a lot of really good tennis courts.) And notice, this has nothing to do, in the way people tend to think of it, with how much longer anyone has to live. There is no reason to think the last three hours of life or the last three days or weeks or months of life are not as potentially valuable as the next thirty years for people who think they have all the time in the world. The only difference is that something good is more likely to occur when there is more time left than with less time left (which is why we tend to oppose suicide in the normal sense, but not always oppose passive euthanasia when someone is dying imminently – we think the healthy person who wants to die has plenty of time and opportunity to find something to want to live for, but the dying person doesn’t), but that is only if all things are equal, and they may not be. There are still potential joys, and profoundly better ways to live and choices to make, left for people who are dying and who have little time remaining. And as long as that is the case, one should want to stay alive. The task in many cases is to help dying persons realize what they have to live for and to help them have ‘their best days’ (including helping them determine what medical treatments will most likely help them experience their best days), and that is not done well by lecturing or nagging. It requires some finesse and understanding of the person (or of people in general) and what may attract his/her attention and in a sense distract him/her from the pain and suffering by focusing on it. You have to lure the person into joys and into thinking about what might make him/her want to live longer in spite of the suffering and pain. I cannot overemphasize the importance of distraction from pain, suffering, and sorrow as 1) a harmless, non-addictive form of anesthetic from them that blocks them, and as 2) if a pleasant distraction, a substitution for them that focuses one’s thoughts and feelings on something joyful instead of sorrowful. Distractions divert attention in a way that can, at least temporarily, minimize or totally eliminate pain, sorrow, or suffering. And although, of course, it is difficult to concentrate on other things when pain or sorrow are intense, in reverse it is also difficult to feel pain or sorrow when one is concentrating on other things. So the trick is to be able to cause the distraction and make it work. One can even do this for oneself sometimes by focusing on something pleasant or challenging a little at first until it starts to take over more and more of your consciousness as you get “into it”. One of the ways this works has been experienced by many people as they may have, say, back pain that they temporarily forget about (and thus don’t have or feel) while they are watching an intense movie or comedy. Intense concentration of another sort is very difficult for most people, but it can be done sometimes by at least some people. It is exemplified by a scene in the movie Lawrence of Arabia, where Col. Lawrence shows some of his friends he can snuff out a lit match by slowing moving his fingers through the flame as he pinches the match with them. One of the others tries it and pulls away, shaking his hand in pain and exclaiming it hurts. Lawrence says of course it hurts, and the guy then asks what the trick is, and Lawrence replies that the trick is not minding that it hurts. (As of this writing, that scene is in a self-contained video clip at https://www.youtube.com/watch?v=TvQViPBAvPk.) On the surface it seems that one cannot help minding pain, but that is actually not true. One can in some sense dissociate it from one’s ‘self’. I don’t know how to explain that other than to say that one can tell oneself that pain is just what is happening in, or two, one’s body and it doesn’t have to make one suffer from it. During a football game a player suffered some kind of ankle injury, if I recall correctly, but played through it and made some remarkable plays that helped win the game. Afterward he was asked how he could do that, and his response was something like “I was only injured, not disabled.” And he knew that playing injured was not, in that case, going to make the injury worse (or cost him more later than he was willing to give up to win the game). Of course it helped that he was able to focus on running his plays, so he had the distraction of that to assist with his desire not to mind the pain and to ‘play through it’. I will return to the discussion about determining the best days and best treatment options shortly, but I want now to take an excursion into the possibility and meaning of not having or being able to have a “good enough” day(s) to make life worth continuing in the face of suffering. In considering what makes one kind of day when one is dying better than another or what makes one treatment allow more good days than another, the natural follow-up question is “What about when no day is good enough to continue to live?”. Dr. Gawande says that, “…we have the opportunity to refashion our institutions, our culture, and our conversations in ways that transform the possibilities for the last chapters of everyone’s lives”, and so: “Inevitably, the question arises of how far those possibilities should extend at the very end—whether the logic of sustaining people’s autonomy and control requires helping them to accelerate their own demise when they wish to. “Assisted suicide” has become the term of art, though advocates prefer the euphemism “death with dignity.” We clearly already recognize some form of this right when we allow people to refuse food or water or medications and treatments, even when the momentum of medicine fights against it. We accelerate a person’s demise every time we remove someone from an artificial respirator or artificial feeding. After some resistance, cardiologists now accept that patients have the right to have their doctors turn off their pacemaker—the artificial pacing of their heart—if they want it. We also recognize the necessity of allowing doses of narcotics and sedatives that reduce pain and discomfort even if they may knowingly speed death. All proponents seek is the ability for suffering people to obtain a prescription for the same kind of medications, only this time to let them hasten the timing of their death. We are running up against the difficulty of maintaining a coherent philosophical distinction between giving people the right to stop external or artificial processes that prolong their lives and giving them the right to stop the natural, internal processes that do so.” (pp. 243-244). I think the distinction between stopping “external or artificial processes that prolong … lives” (generally called passive euthanasia) and “natural, internal processes that do so” (i.e., active euthanasia) is not helpful. You are no less responsible for ending the lives of people by turning off their underwater diving air or by stopping their airliner engines at 35,000 feet than you are if you were to shoot or poison them. Unnecessarily discontinuing or removing what easily keeps people alive is no less killing them than is inserting something into their system that is fatal. The means by which you help someone cut short their life is secondary to whether it is right to help them cut it short or not in the first place. If it is right, then the means must be the most humane, but if it is not to (help them) cut short their life, then using humane means does not justify doing it. I will give more reason for that in a page or two in a discussion about euthanizing dying and suffering pets by active versus passive euthanasia. But I also discuss it in Active Vs Passive Euthanasia: Moral Equivalence or Not? Philippa Foot Vs James Rachels. But eschewing or terminating a treatment that makes your (quality of) life significantly worse than it otherwise would be, even if prolonging it, is not the same thing as refusing, rejecting, or terminating a treatment that simply prolongs your life whose quality is not good, but the treatment does not make it worse. Suppose, for example, you have two treatment options where one has a somewhat greater chance of prolonging your life but making it significantly more miserable than the other which may be 20% less likely effective but will not make it worse. Surely, opting for the second treatment is not to be committing suicide or even trying to shorten your life. And I see no reason to believe it is opting for suicide to pass up the first treatment even if there is no second treatment, but life with the treatment is worse than life without it, even if life with it is longer. And clearly, if someone healthy passes up exercise that might prolong his/her life in order to do something more important to him/her with that time, that is not choosing euthanasia or suicide either. The question of whether life is worth continuing or not is a different issue from whether something risky is worth doing or not worth the risk. And it is a different issue from the most reasonable way to terminate life if it is determined to be right to end one’s life prematurely. We accept that animals such as cats, dogs, and horses can have their lives terminated to prevent suffering, but as of this writing many people do not accept that for human beings. I for one, do not accept it for human beings, not because I believe in the absolute sanctity of life (I don’t) but because I think that some suffering can be worth enduring and so it is not suffering itself that is a sufficient or definitive justification or grounds for euthanasia, even voluntary euthanasia, but only unredeemable suffering, the endurance of which would be totally worthless, totally pointless and valueless. But there are at least two relevant differences between humans and lower animals in that humans can anticipate likely having an experience that will make enduring the suffering worthwhile and lower animals cannot likely anticipate the future or have any understanding of something making suffering worth enduring. As one of my student said, it is perfectly understandable that a dying suffering person might want to hang on to know about the birth of a grandchild and be able to see the baby, but if you kept your cat alive while suffering till it saw a litter of grand-kittens, it would probably ask, if it could talk, “What; you made me suffer an extra week to see this? What do I care about this!?” Moreover, imagine taking your pet to the vet who says “S/he is dying and suffering terribly. We should put her/him down. You can do that at home yourself or leave her/him here. We simply need to stop feeding him/her or giving him/her water, and that will hasten his/her death, naturally. In the old days, we used to inject animals with something that terminated its life immediately painlessly, but that is now considered to be murdering the animal, whereas just letting it starve or dehydrate to death is not.” We would balk at that, because if it truly is time for the animal’s life to end rather than prolong its suffering, it would be wrong not only not to end it now but to make whatever time it does have left naturally be even worse quality than the condition it is in that made the vet determine its life is already sufficiently bad to warrant helping it die sooner in the first place. The fact there are potential joys for many different people does not mean that life always has something available to each person that can make that person’s continuing to live worthwhile. Some people simply run out of things that they can enjoy or appreciate, or they lose the ability to enjoy or appreciate anything, and nothing and no one can rekindle their ability to anticipate or find any joyful significance in any experience. I believe that is more rare than we tend to believe; and I think we often give up on trying to nurture a spark of interest because we don’t know how to do it, but I think there are cases where probably nothing can make someone’s life worthwhile to/for them. Often we mistakenly think in terms of severe physical disability in this regard, but studies show that even paralyzed people are as satisfied with their lives as able-bodied people are satisfied with their own lives. We tend to think of physical disability, particularly paralysis, as being an awful way to live or too awful to continue to live, but those who face it don’t find it so awful as able-bodied people imagine it, and they don’t normally find much less about what makes life worth continuing to live than able-bodied people do. Paralyzed people generally rate the quality of their lives virtually as high as able-bodied people rate the quality of their own. Or consider a confining illness or injury, which would normally be considered a bad thing. In some cases it can actually be a blessing to the person suffering it, particularly but not necessarily only, if it is temporary though lengthy. A confining condition that is ‘socially acceptable’ and viewed sympathetically by others can give one the time and focus to do something one might otherwise not be able to do without the reprieve from other responsibilities or interests. That could be to make the best of a bad situation. And if Dr. Kalanithi, for example, had been given two years to live, time which he used to write his book instead of doing research or surgery while also trying to write in his spare time, and if then his cancer miraculously vanished, leaving him fully healthy, and thus getting to, but also having to, resume his previous responsibilities and interests, he probably would still be grateful for the time off to write that the ‘two year’ prognosis afforded him, despite its sadness at the time. Moreover, in some cases the shrinking of one’s possibilities causes and/or requires a change in attitude or appreciation. A team that goes into a football game not wanting to tie might be thrilled by getting a tie if they score a touchdown and a two-point conversion in the last second of the game. Diminished opportunities and hopes can lead to greater appreciation of smaller triumphs, kindnesses, and other joys or they can lead to resentment that small pleasures and triumphs with lower expectations are all that are left. Tennyson expresses the former almost perfectly in these excerpts from his poem “Ulysses” (with one addition by me to better fit the context here, with my apologies to Tennyson): … I will drink Diminished opportunities of one sort can also contribute to desirable achievements of another. I used to believe that a perfect example of utilitarian decision-making involving juxtaposing probability with value of the different options was that although normally in a football game teams elect to kick for one point rather than go for a two-point conversion, or they chose to ‘settle for’ a field goal on fourth and eight from 30 yards out because scoring fewer, but more likely, points was better than not scoring at all. However, I thought it was most certain that at the end of a game with time left only for one play, that a team that just scored a touchdown leaving it down by two, should go for two points rather than one, since the value of two points was not just worth twice the value of one, but worth infinitely more at that point in the game because it was the difference, not just of one point, but between a possible tie and a sure loss. Similarly with only time left for one last play in the game, surely no team down by five would elect to kick a field goal for three points instead of trying for a miraculous touchdown, since a field goal would still give them a loss, and a remotely possible opportunity for a victory was better than a sure loss. However, one day it occurred to me there is a kind of possible situation where the team would kick the extra point or the field goal even if it meant a sure loss as opposed to a possible tie or victory – cases in which the team’s season was already lost even if they won this game, but where in this last game of it, a beloved kicker had a chance to set a new record by kicking the extra point or the field goal and the team wanted to give him that opportunity and wanted to be a part of his success and his breaking the record. There are all kinds of factors that can go into determining which options open to one are valuable or more valuable than others. Now, it is my view at this time that a person who wants to die (or in the case of someone who cannot communicate his/her wishes to us, would most likely want to die under the circumstances s/he is in), should be allowed to (or helped to) if and only if it can be pretty certain that his/her circumstances make it impossible that anything which can likely happen in the time s/he has left to live will make the suffering s/he is experiencing worth it to him or her to endure. That means that the best effort has to be made to seduce the person into wanting something[4] they will have to live to experience, by the people most likely able to do that (which is not likely going to be clergy or psychiatrists, unless they are gifted at this apart from their professional training, or perhaps are great friends of the patient), and if and only if that effort fails, then it will be right to help or let the patient die. Life should not be ended if there is anything to make it be worth whatever pain or suffering one might have to endure. But if there is nothing that can make a person’s life and suffering worth continuing and have value that is likely to be possible within whatever lifespan they have left, then either euthanasia or suicide would be right if they are suffering terribly and want to end their life. The difficulty is determining when that is and convincing someone who thinks they have nothing to live for that they are wrong, if and when they in fact are wrong. The amount of time left to live is not necessarily relevant, or the most relevant factor, since the last three days of life are no less important than any other three days. As I tell my students, they don’t go back to work early from their vacation just because there are only a couple of days of vacation left and there is no point in utilizing them – unless they hate being off work and prefer their job to free time. Determining when life (or an activity in life) is not worthwhile is not necessarily a simple calculation. Sometimes it involves the most valuable use of your time, which may vary under different circumstances. Suppose you attend a play or movie that turns out to be long and boring but that you have sat through, hoping it would get better, until now there is an intermission with maybe 20 minutes left to go in the show that gives you the opportunity to leave without being noticed. The last 20 minutes might or might not give an ending that in some way makes up for or redeems the time you have already spent, whereas if you leave, you will have wasted that initial time for sure. So that last 20 minutes now has more potential value for your staying rather than leaving, unless you know you have something better to do with it, like going off with someone you met at the performance with whom you have an immediate mutual attraction and that person wants to leave too. However, if you knew ahead of time the show would be boring for as long as it was (and that you would not likely meet a person there you are attracted to), you probably would not have gone, because you likely could have better spent the whole amount of time doing something else. Basically, in any case where resources, whether time, money, labor, etc. have already been somewhat lost or wasted, it is difficult to know whether to expend more or the remaining resources trying to get at least something out of what was already used. It is not always easy to know whether those remaining resources can be better utilized elsewhere or not, and there is a pull between salvaging something from what is lost and not wasting more. Or consider any situation where one has to choose between saving the life of an infant or an older person. One argument is that the infant should be allowed to live to experience some of the most important joys in life that the older person already has enjoyed. Other people, including myself, think that time already invested in growing up, which I think is difficult and often sorrowful, deserves to have a payoff of the joys of adulthood that are, I think, much greater than most of the joys of childhood, because they are harder earned. I see childhood as putting in a lot of painful learning, though with some joys along the way. And I see certain moments of adulthood as being overall greater in joy and satisfaction (even if the joy of learning to ride a bicycle is the potentially single greatest joy anyone can have and occurs in childhood). Moreover, I see dying in infancy not only as missing joys, but missing all the sorrows, fears, and other sufferings of life. While one misses playing in the snow or feeling the sun on the first warm day of spring, one also misses having to give school and work reports or do science fair projects, fear tests and maybe even get poor grades, suffer disheartening sports losses, disappointments in love, embarrassments and humiliations of all sorts, etc. Now, admittedly it is difficult to know over the range of a whole long life available which sorrows might be worth which joys, and sometimes it is easier to make that determination when life is shorter and the opportunities for both suffering and joy are more narrow and defined. And it is also the case that the more time, energy, and effort already invested in something skews the balance, since, for example, while we lament a miscarriage or loss of infant life as a shame for missed opportunities for it, we don’t normally lament the same missed opportunities of (additional) children never conceived, never thought right to be conceived and not desired to be conceived because they would not have had sufficient joy compared with suffering to make it right to conceive them. The criteria for justifying continuing something already begun is often different from the criteria for justifying beginning it in the first place. But time remaining also can be either a simplifying or a complicating factor. The kind of purpose will depend in part on the likely length of time left. Dr. Kalanithi wrote, “If I had some sense of how much time I have left, it’s be easier. If I had two years, I’d write. If I had ten, I’d get back to surgery and science.” (pp. 130-131) But that is true for healthy people, even young ones too. The conventional mistaken advice given is “Live each day as though it may be your last.” A teenager on the late 1970s TV show Eight Is Enough pointed out the flaw in that advice when she responded “I tried that once and got grounded for three months.” The difficulty is that without knowing the future or its length, you have to plan for it in case you live to meet any given stage of it. You have to invest time, energy, and money into a future that may or may not arrive, when it would certainly be more fun to spend it on a shorter term (particularly an immediate) payoff if you knew there would be a much shorter or no future. Also, presumably the reason Dr. Kalanithi would choose to get back to surgery and science if he knew he had ten years remaining rather than just writing because he only had two years, is that with ten years he could still write the book he wanted to in his spare time from surgery and science. The correct advice is that you should live each day as though it might be your last and also as though it might not be your last. Of course, that advice is not real helpful, other than as a reminder you should neither postpone all pleasures till later nor pursue them all now, but need to try to pace yourself and your resources for greatest or most reasonable benefit over time, though you have to do it at an indeterminate pace. For those people who have a ‘bucket list’ (that is, one that is different from just their normal everyday ‘list’ because it is somehow predicated on having little future remaining), knowing when it is time to begin checking off the activities on it, is important. The concept of a bucket list is itself somewhat interesting. I can see, if one had no other responsibilities and no future life left to have to save up money for, that one might spend lots of money taking a trip to an expensive destination one really hoped to visit some day. But I myself cannot see doing something like skydiving because I only had a week left, when I wouldn’t do skydiving otherwise, since I wouldn’t want to give up that week any more than I want to give up an unknown amount of time, and I don’t want to die (or even break a leg) by hitting the ground too hard or in the wrong way from any kind of height. Since I am not a thrill seeker or ‘adrenaline junkie’, the only thrill of skydiving seems to me to be not being killed doing it, and I have had that thrill every day of my life, and plan to continue having it. Sir Walter Raleigh’s response poem to Christopher Marlowe’s is a great example of the factor time and its vicissitudes can play in making choices about what to do:
It is not that life is good no matter what, so the sanctity of life is not a correct principle, unless you want to hold that it is right for God or nature to be cruel, and that we should endure all suffering no matter what, and make all others endure it too if they are unfortunate enough to suffer (even if they are innocent, as in the case of babies or children, and even many adults). That view just seems too callous and indifferent to people’s suffering, even if one could maintain it. (And notice that the sanctity of life principle is not necessarily a religious one. One can hold that life is of absolutely ultimate value because of the seeming miracle of consciousness, no matter how it comes about.) However, the quality of life principle also either fails or at least needs explaining. Many seem to take that to mean that life may be terminated when the quality becomes terrible, but that troubles them – and it should -- because we should not be willing to die just because our circumstances are not good. Most people face circumstances at least from time to time that are not good. Most people suffer at some time or other. Many, if not most people, have a “negative balance” of more bad or boring times than good times in their lives, and the intensity of bad times is often worse, in some way, than the intensity of good times. And yet, quite correctly, we don’t feel that is reason to commit suicide or to hasten our own deaths or the death of someone else. We need to examine the idea of “greatest balance of good over bad consequences,” because, as just said, it may not, and perhaps usually doesn’t, mean there will be a greater amount of good times than bad or a greater amount of joy in terms of intensity than suffering in terms of intensity. What I am suggesting is that another way to think of this balance, and the one most appropriate for end of life issues, is a qualitative sense in which good “outweighs” the bad, rather than a quantitative sense, and in particular for end of life issues, whether the good things are sufficient to make the bad part worthwhile enduring. The easy cases, which most tend to discuss, are cases of full or great recovery from some terrible condition. But the cases normally overlooked in medicine and society in general are the cases where there is not going to be recovery, where the patient will die, and yet some minutes and some experiences near the end may be precious enough to the person to, in the sense we are talking about, make enduring the suffering worthwhile in order to have had. If so, then in this sense, there will have been a greater balance of good than bad, even though the balance will be one of quality in some intangible sense, rather than of time or of intensity. Hume and almost everyone else in discussing these sorts of cases think only of the pain and suffering, and not the benefit for the patient of enduring it. If people think of benefits at all, they tend to think of the benefits for the friends and loved ones of the patient for prolonging the patient’s life. But there can be benefits for the patient too. If you think only about the pain and suffering, that is like evaluating a purchase only on the basis of its cost, and not on the basis of what you might receive for the cost in relationship to it. I want to try to show here that either the quality of life argument fails or that it needs to be understood in a way different from how you and most people understand it. The semantics can go either way – about whether I am suggesting a different principle altogether or just a more explicit, particular interpretation of the quality of life principle. Which of those two ways you choose to characterize this is not important. The idea is what is important. And the idea is that as long as there is anything that can make our continuing to live be “worthwhile” to us, even in the face of adversity and suffering, then life is worth holding onto. If a time arises or conditions arise that it is no longer possible for anything we are likely to experience to make up for the suffering we have to endure, then it is permissible for us to die if we wish to. [Wanting to die, or at least being justifiably willing to die, is a necessary condition along with their being nothing possible for which to live, because if a person does not want to die or be willing to die (say, to save others), we shouldn’t kill him/her even if s/he has nothing worth living for. It would violate the person’s right to life to kill him/her if s/he does not want to or is not willing to die; and it would be murder, except in cases of self-defense, defense of an innocent third party, in deserved capital punishment, or as a just act in a just war. But although a person’s desire to die is a necessary condition for euthanasia to be right, it is not sufficient, because one can mistakenly want to die, as exemplified by attempted suicide survivors who knew they made a mistake just after they made the attempt, as in the guy who survived a jump from a popular suicide bridge and later said he realized the second it was too late to stop his jump he didn’t want to die, or as in people who have lost sight of some interest that could entice them into living, and as in people who were persuaded or forced to continue living when they preferred to die and who later appreciated it and were thankful and grateful to have continued living. Sometimes people also are afraid to do what is necessary to live longer, and they have to be helped overcome that fear, not just told they should not be afraid or told they need to do the thing because they ought to live. Going with a friend or loved one to procedures or being with them at the right times, can help overcome the fear or the sense of isolation. Or to put it in terms of the right to autonomy, autonomy as a deserving person’s decision to live is an absolute right, but as a decision to die, autonomy is only a prima facie right, not an absolute one, as in “friends don’t let friends drive drunk even if they are only going to hurt themselves” and as in the fact that you are not violating anyone’s rights if you prevent them from committing ‘garden variety’ suicide.] But we should also not let someone else die (nor decide to die ourselves), if something is possibly worthwhile and in some sense “redeems” for them (or ourselves) all the suffering they (or we) have to endure. It does not matter how brief or how small a portion of our total quality (or lack of quality) of life the redeeming or worthwhile experience is, or how unimportant it might be to others. One student in the past came closest to seeing this principle when she pointed out about the case of a dying woman with a DNR order whose grandchild was about to be born. The point is that grandchild’s birth might make it worth reviving her for to show her the baby or tell her about it even if it means prolonging her suffering. It is not just the quality of our experiences but the meaning and significance of them to us that matters. One might call this the “significance of meaningful or worthwhile experiences” principle, because it is not just about how much is good in either absolute quantity, intensity, or in terms of proportion of good to bad in our lives, or how objectively good it is (e.g., wealthy people who have “everything” often are depressed and commit suicide, because they are missing something meaningful to them), but about how important or significant or meaningful something is to the person. Significance or meaningfulness is a quality of goodness that needs to be taken into account in balancing good and bad; and it is different from intensity, duration, or quantity of goodness. In some ways it might be the most important aspect of goodness that one needs to compare to the burdens in life, because a small amount of significant goodness can (and does for most people) override a large amount of burdens or even intense suffering. Now what might make one’s suffering worthwhile is going to be different for different people, and that is where individual preferences come in, but there are all kinds of things that can be of value to people, whether it is finding out if your team wins the Super Bowl to just the touch of a loved one’s hand or the sound of their voice, and knowing that they care. It can be the kindness of a stranger (or nurse or hospice worker) or experiencing closeness with God or nature or with feeling and appreciating what one person referred to as “the benign indifference of the universe”. It can be doing one more kindness for someone else. It can be falling in love. It can be watching the Comedy Channel and hearing some comedian characterize in a funny way something that has always otherwise troubled you or made you angry or upset and that you thought no one else experienced or could understand – and yet here is someone who not only experienced it and understands it but is able to portray it in a light that makes you laugh really hard at it. It can be seeing some work is finally published or recognized or it can be finding the solution to some problem that is bugging one. If one thinks, mistakenly, that life has to be predominantly good or have length into the future in order to be worthwhile, that perspective makes one miss noticing a lot of good that actually makes one’s life worthwhile. If one is attuned, however, to all the possible things that happen that can make up for all the bad moments or the most terrible suffering, then there is much more of a chance one can find reason to hang on and to live each moment one can. [“The Right to Physician-Assisted Suicide” is a paper that deals with this also from a practical angle.] And now an excursion into one often-pointed out seeming inconsistency, even unfairness, in those opposed to active euthanasia for people, while allowing it to be a standard practice for animals, as in putting pets to sleep and as in “they shoot horses, don’t they?”. Since the issue is usually raised about the seeming unfairness that we euthanize animals, but not people, I want to address that here because it also sheds more light on the ideas above. Some people think it unfair to animals that we end their lives early, while others think it unfair to humans that we don’t end their suffering early. The question is simply about applying the principle to animals: is there anything that makes the animal’s life worthwhile despite its suffering – anything that can make it worth continuing to endure the suffering likely to come? First, some people say we can’t know what animals want or how they feel, because they cannot tell us their wishes in the way people can and they cannot tell us whether their lives are worthwhile in the way people can. They say it is therefore unfair to make the decisions for the animals. But those who have had experience with pets or other animals point out you can pretty much tell how they feel by the way they are acting. Some people even think you can tell by their expressions, at least in conjunction with their behavior. But for various reasons it does not matter in this regard that people can talk and animals cannot, since 1) we have to use our judgment anyway about whether to help or let them honor their wishes, and 2) people are often mistaken about what they want. Even regarding people, if they tell you what they want, that doesn’t mean you have to believe they are correct or wouldn’t change their mind or that they really know what they want. And this is not just in regard to dying, but even simple things, as when you know your spouse or friends must be hungry even though they say they sincerely say they are not – so you serve them some food, and they smell it or take a bite and then say “Gee, I guess I was hungry; this is great” and then they devour it. Of course, you need to take what people say into consideration and normally assume they are right about themselves, but there are times that is not the case and you have to understand that and sometimes, depending on the circumstances, not honor what they say – as in “no, I’m not too tired to drive” or “I can drive; I haven’t had too much to drink.” Moreover, you can’t assume it is unfair to euthanize the animal who can’t talk, unless you are able to show it is better and more fair for the animal to suffer than to die, and that you are not therefore being unfair to it if you make it continue to live and suffer instead of helping it die mercifully. Some people have the idea that living at any cost is better than death, even though that is only a prima facie presumption and there are clear cut cases where it is at least highly doubtful if not clearly false. The “fair” thing to do for the animal is to do what is best for it if you can, and if euthanizing it is best for it, then that is the fair thing. Making it continue to live with irredeemable and unnecessary suffering would be the unfair thing. But there is something else that I believe is even stranger about the argument that it is unfair to animals to euthanize them because they can’t tell us what they want, whether they want to live or to die, given their suffering and the likely outcome. For even though dogs, for example, clearly have some sense of cause and effect and anticipate a certain amount of future happenings (as shown by their sitting near their food bowl near the usual feeding time, or their getting excited about going out when you get up to get their leash, or anticipate your coming home when they hear you approaching from outside, etc.) there is no evidence animals (at least animals such as dogs, cats, horses, and other “lower” animals) have some sort of long range sense of cause and effect or planning or that they have any sense of their own mortality or even what their own death is. Yes, dogs might look forward to being fed turkey they smell cooking, but they don’t likely look forward to Thanksgiving or to your making turkey next week. Dogs don’t likely look forward to retiring or to spring. Dogs know it is cold and may wish to get warm by going inside, and they may bask in the sun when it finally starts to warm up, but they hardly seem to look forward to spring or to anticipate it. There is nothing for the dog to look forward to or expect to experience, or actually experience because of its significance to the dog, that would redeem its suffering or make it worth enduring. Similarly with the previously mentioned suffering, dying cat and its grand-kittens you kept it alive to see. This is not to say such animals have no knowledge or desires or instincts. They do. So you have to be careful in distinguishing what an animal likely wants from what it doesn’t and from what it likely cannot want because it doesn’t understand that there is something too want. Those who say dogs cannot tell us what they want about continuing to live or not or whether their suffering is worthwhile or not, seemed to miss the bigger point that the reason they can’t tell us whether they want to die or to continue to live, is not because they can’t talk or write or blink their eyes in code, but because they can’t even know there is some sort of choice – they don’t even understand about dying versus continuing to live and suffer. If that is the case, then for sure we have to make the choice for them, and so we need to make that choice based on best available evidence about what is best for them. Now it seems to me that it is pretty clear we can tell when an animal is suffering; they tend to evince the same kind of pain behavior people do (and we can tell when people are suffering even before they tell us they are). They shriek in pain, they cry or whimper, they limp with obvious hardship, not with zest or enthusiasm, they have unhappy expressions, they may be unwilling to try to do something they know they can no longer do, they are often listless, they may give an appearance of frustration, disappointment, unhappiness in general. But we also know when they don’t mind that something is problematic. A dog with arthritis can still show excitement at greeting its owner, even though it can’t jump up on him/her. It may hobble around limping or dragging a leg but still be frolicking about outside doing it. You can tell when a dog for instance is happy even though injured or hurting. And there is no need to euthanize such a dog then. It would be wrong to do that. You can even tell when an animal is hurting so bad that it is suffering terribly, and yet it either goes off to lie down and you can tell it takes some solace in that or particularly if it comes to you and just wants to lie near you or be held by you. There is no need to euthanize it at that point, because it is clearly feeling some sort of love and affection that is somehow making its suffering worthwhile – at least giving the strong appearance of that. Young children give the same sorts of appearance sometimes, and you may even remember as a child being really sick, but taking some comfort in being held or just being left alone in bed to go to sleep or to read – without any thought about dying or sometimes even feeling better; just trying to reach some sort of comfort level, which was sufficient for you at the time. My wife had a grandmother who said “Things never get so bad you can’t just go lie down.” There is a point to that, but it is not always true, and you can tell when a child or adult or an animal cannot even find comfort in lying down or anything. And that, it seems to me, is when it is right to euthanize the animal but not necessarily the human, because the animal, unlike the human, cannot have anything to look forward to that would make such suffering worthwhile, and nothing (given the animal is dying) will likely happen in the immediate future that would make the animal grateful to have lived to see it. (We are not, after all, talking about euthanizing a dog that is merely temporarily sick.) If you euthanize a human you may be robbing him/her of some anticipated or worthwhile goal or desire it wants to (live to) experience, but you are not doing that when you euthanize an animal – presuming it has evinced no anticipatory behavior about such an event. So to answer the question of whether it is wrong or unfair to animals that we euthanize them or to people that we don’t, I am claiming it would be wrong and unfair to euthanize either an animal or a person if they still have something to live for and/or still want to live, but not if they don’t. And animals reach the state of having nothing to live for and not having a desire to continue to live “sooner” (in some sense of sooner) than people do because animals do not (seem to) have any sense of anticipation, long term planning, knowledge or fear of their own death or impending mortality, etc. that humans do. Again, this has been about animals such as dogs, cats, horses, etc., not necessarily dolphins, chimps, etc. that may have the mental abilities to contemplate the future, make plans, have long range desires, etc. Insofar as they do, they should be treated more like humans; if not, then more like dogs and cats. But the extent of their mental capacities in that regard is a factual question, not a moral one. The moral principles are the same for all – for both humans and animals, so there is no inconsistency; but the factual circumstances will give different outcomes using the same principles, just as when you are playing poker, your principles for how and when to bet will be the same for all hands you are dealt, but how much you actually bet and when will depend on the specific hand you are dealt, when you apply those principles to it. It should be pretty clear from all this that making choices about what is best for us involves more than just the peak or end points that we might remember or dwell on of a past experience. The Significance
of All the Above for Choosing Treatment Options The role of medicine should be to help people have the best health they are reasonably willing to try to achieve in order to have the most worthwhile reasonable life they desire in the time they have left, which shortens with age and with various conditions, particularly ones considered terminal. Also, age, illness, and injury generally cause relatively more suffering and pain, which people then need more help to make them be worth enduring. This is particularly important when the cost of enduring physical pain, though possibly great, is less than the consequences of trying to minimize or eliminate it through things like drugs that have less acceptable side effects than enduring the pain or through surgeries that have unacceptable risks. This requires knowing the possible and likely outcomes of all the treatment and non-treatment options and what they might mean for the patient reasonable sense of best spent remaining time, whether long or short, so it applies to the practice of all medicine, not just old age or terminal conditions. So-called ‘end of life’ conditions are just special cases with heightened awareness of more immediate consequences and narrower, relatively less attractive or desirable, options and outcomes. Physicians need to understand (whether on their own or with assistance of someone who can explain it to them or whose understanding they trust) what might reasonably make a patient -- whether one who is precariously premature, terminally ill, or acutely or progressively disabled or infirmly aging -- better or worse off, not just physically but in terms of the quality and value of their life to them. Physicians at least need to realize that the best biological
care is not necessarily the best medical or patient care nor the most
reasonably desirable option to the patient. It also requires (and this is not necessarily,
and certainly not solely, within the scope of medical care) helping the patient,
where possible and feasible, have coping skills such as good distractions from
pain, a perspective on his/her condition that is most tolerable, appreciation
for the pleasures and joys remaining, and potentially achievable good purpose(s),
particularly one(s) which are gratifying and fulfilling to pursue even if not
ultimately achieved. References: Churchill, W. (1898). The Story of the Malakand Field Force, London. Retrieved from http://www.gutenberg.org/files/9404/9404-h/9404-h.htm Darrow, C. (2005). The story of my life.
Project Gutenberg of Australia. Retrieved from http://gutenberg.net.au/ebooks05/0500951h.html Gawande, A. (2014). Being mortal: medicine and what
matters in the end. New York: Henry Holt and Company, LLC. Hume, D. (1779). Dialogues concerning natural religion. London. Kalanithi, P. (2016). When breath becomes air. New York: Random House.
[1] To
make I am doing justice to their reasoning and the beauty and power of the
prose of both Dr. Gawande and Dr. Kalanithi, I am quoting more than the bare
minimum references from them. Since I am
trying to build on what they say, but with need to criticize some of it, I believe
this falls under the fair use copyright exception, and I have tried to judge
what is necessary and sufficient to give them due credit and put my own
observations in the proper context of their positions quoted for accuracy,
without infringing on their rights or sales.
I highly recommend your reading the two books cited in their
entirety. The passages I quote are only
a small sampling of their insights and their eloquence.
[2]
The calculations can change as the (potential) future shrinks or expands in
length of time. E.g., surgical repair of
a partially torn rotator cuff that is not immediately life-threatening would
not likely be something advantageous to the patient who is dying soon of
something else, whereas it might be a reasonable choice for an active, healthy,
young person. There is no need to risk
what little time you have left you could be using to enjoy something else in
order to have the benefits of a repaired rotator cuff for that same short
amount of time, whereas a long time of rotator cuff damage and pain that could
be avoided by successful surgery would be worthwhile. One or a few small pleasures can make a short
time of suffering worthwhile but would be insufficient for a long lifetime of
suffering or boredom. In each kind of
case, different parameters may have more weight than they do in other cases,
and each needs to be considered. Also
any return on past investment of time and energy is better than none, but one
would not invest that same time and energy for just any (small) return if there
were better things to do with that time and energy (which would yield a more
likely better return).
[3] The pressure by friends, family, and loved ones becomes a kind of self-pressure in part also, because you hate to disappoint relatives and friends who don’t want to see you die sooner than necessary because they don’t appreciate your suffering. And particularly because you hate to let them know their friendship and love are not sufficient to make the suffering worth enduring – just as you don’t want to go to a wedding, especially a destination wedding, with them or shopping or camping for the weekend. Companionship is not always sufficient thrill for enduring something unpleasant. There are times it is appropriate to fantasize saying that in the Bette Davis style shorthand: “Sure, I love you, but… I’m going to wash my hair.”
[4] Things
we want to do or be able to do and things we want to get, or have a chance of
getting, or want to have happen, or have a chance of happening, especially
things we think we deserve. And getting
or doing some of those or the opportunity to get or do them needs to
subjectively make enduring the other things worthwhile. It is not about life being worthwhile, but
about whether enduring suffering through the bad things in life is worthwhile. One example from a student was that if his
mother were dying or invalid, she would probably take great pleasure in
whatever time she had left helping her children and grandchildren and their
spouses learn to cook well their favorite foods she always prepared for them from
her own recipes. She had always loved to
create recipes, loved to cook, and loved to watch her family enjoy what she
served them. This way she could ensure
their joy from her creations continuing.
[i] (1) There is a ship in the harbor with a very long rope-ladder hanging overboard whose rungs are 8 inches apart. At the beginning of the tide's coming in, three rungs are under water. If the tide comes in for four hours at the rate of 1 foot per hour, at the end of this period, how many rungs will be submerged? The answer is not nine, but "still just three, because the ship will rise with the tide." This does not demonstrate respondents do not understand buoyancy, only that one can be tricked into forgetting about it or ignoring it. (2) Three men went into a hotel in 1927 and got a suite of rooms for $30 total, which they paid in advance in cash, each man contributing $10. After they went up to the room, the desk clerk realized he made a mistake and that the suite was only $25. He gave the bellhop $5 to take back to the men. The bellhop did not know how to divide the money evenly among the men, so he merely returned $1 to each of them and kept two for himself. That meant the men paid $9 each for a total of $27. The bellhop kept $2, so that is $29. But there was $30 to begin with, so what happened to the other dollar? This tends to be an extremely difficult problem --psychologically-- though it has an extremely simple answer. The money paid out must simply equal the money taken in. $27 was paid out (ultimately); $2 of it went to the bellhop and $25 went to the desk. You must subtract the $2 the bellhop kept, not add it back to the amount the men paid out. There is no reason to add the $2 to the $27 other than to get a number close enough to the original $30 to confuse the listener into thinking something is wrong and that $1 is unaccounted for. People who cannot solve this problem, generally have no trouble accounting for money, however; they do only when working on this problem. (3) The following problem is difficult the more calculus you know. If you know no calculus, the problem is not especially difficult. It is a favorite problem to trick unsuspecting math professors with. Two trains start out simultaneously, 750 miles apart on the same track, heading toward each other. The train in the west is traveling 70 mph and the train in the east is traveling 55 mph. At the time the trains begin, a bee that flies 300 mph starts at one train and flies until it reaches the other, at which time it reverses (without losing any speed) and immediately flies back to the first train, which, of course, is now closer. The bee keeps going back and forth between the two ever-closer trains until it is squashed between them when they crash into each other. What is the total distance the bee flies? The computationally extremely difficult, but psychologically logically apparent, solution is to "sum an infinite series". Mathematicians tend to lock into that method. The easy solution, however, is that the trains are approaching each other at a combined rate of 125 mph, so they will cover the 750 miles, and crash, in 6 hours. The bee is constantly flying 300 mph; so in that 6 hours he will fly 1800 miles. (One mathematician is supposed to have given the answer immediately, astonishing a questioner who responded how incredible that was "since most mathematicians try to sum an infinite series." The mathematician responded with astonishment of his own, "but that is what I did.") It is not that mathematicians do not know how to solve this problem the easy way; it is that it is constructed in a way to make them not think about the easy way. (4) A similar problem is: You have $100 in the bank. One day you go to the bank and withdraw $50, leaving you $50. On another day, you go in and withdraw $25, leaving you $25. On your third trip to the bank, you withdraw $10, leaving you $15. Then you withdraw $8, leaving you $7. Then you withdraw $5, leaving you $2. Then you withdraw that $2, leaving your account empty. The following table shows what you withdrew each time and what balance remained after that:
But, as you can see the two columns don’t add up right. The first one adds up to the $100, but the second one only adds up to $99. What happened to the extra dollar? The answer is nothing happened to it; there is nothing
missing. The balance column has nothing
to do with how much money you withdrew altogether, and the only reason it comes
out close to the original $100 is because it was constructed to do that. If you had taken out all $100 to begin with,
the balance column would have been zero; and if you had taken out $1 at a time,
there would have been 99 entries in the balance column, starting with $99, then
$98, then $97, $96…, $3, $2, $1, 0, adding up to something like $4950.
[ii] The captions in the following photos say: It is disproportionately insensitive and unreasonable to esteem and envy the driver of one of these wheelchairs simply for having it, while disregarding or pitying the operator of the other simply for using it. Both sets of wheels are made to extend the range of mobility for those who need to go further than they can walk. 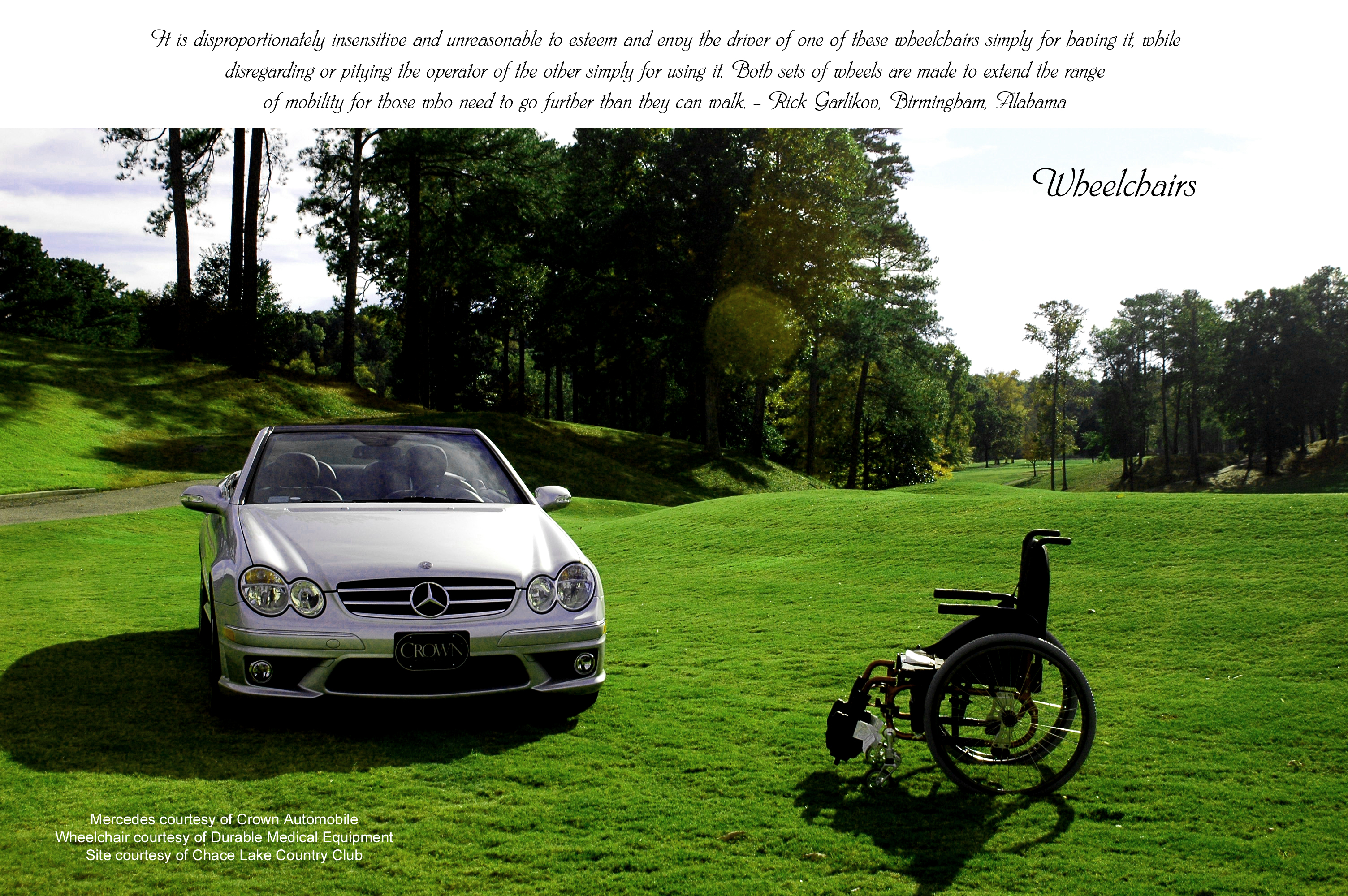
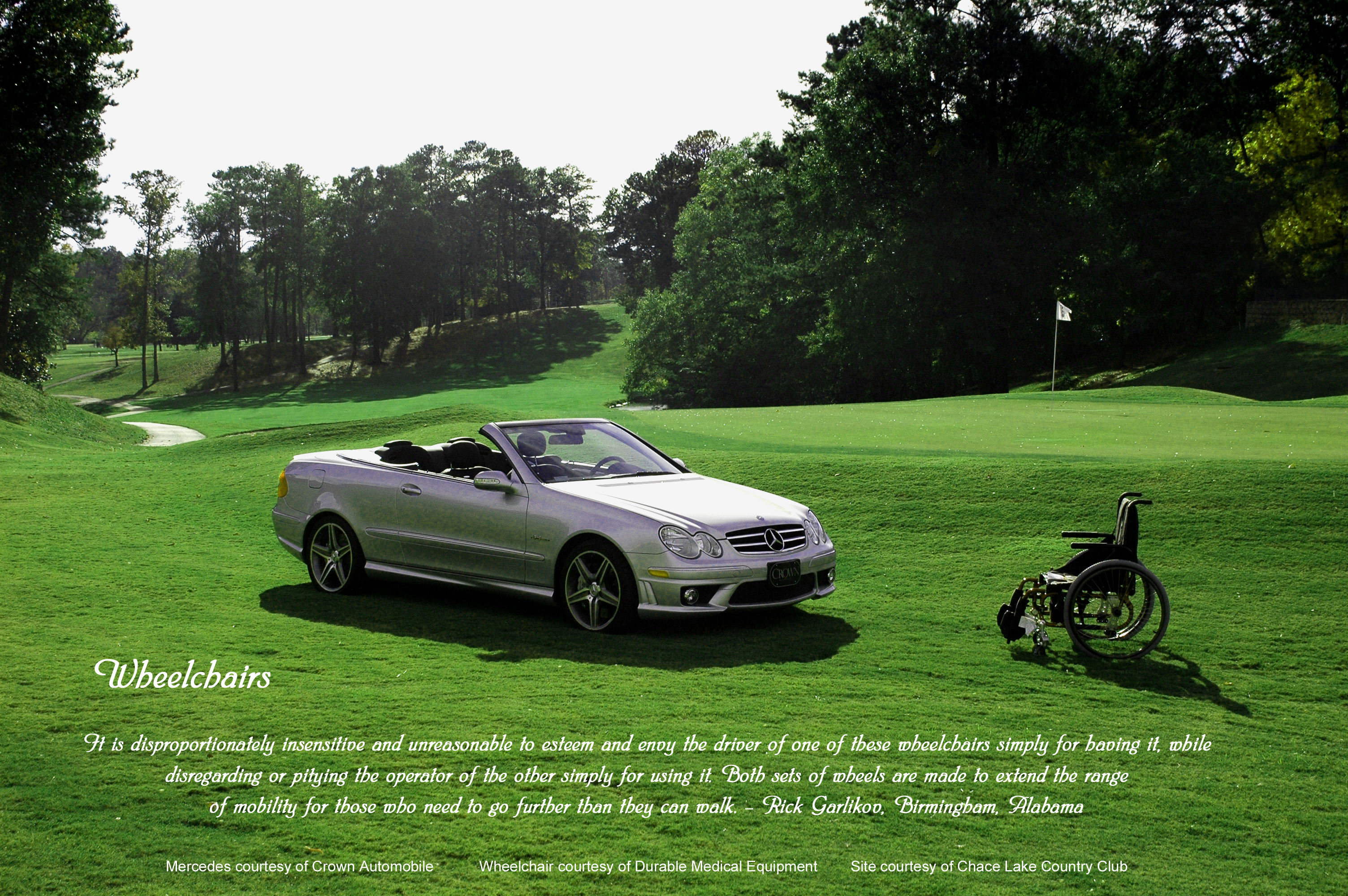 |